The document provides information on the thyroid gland, including its anatomy, histology, physiology, pathology, and disorders. Some key points:
- The thyroid is one of the earliest endocrine organs to develop. It is located in the neck and weighs 15-25 grams.
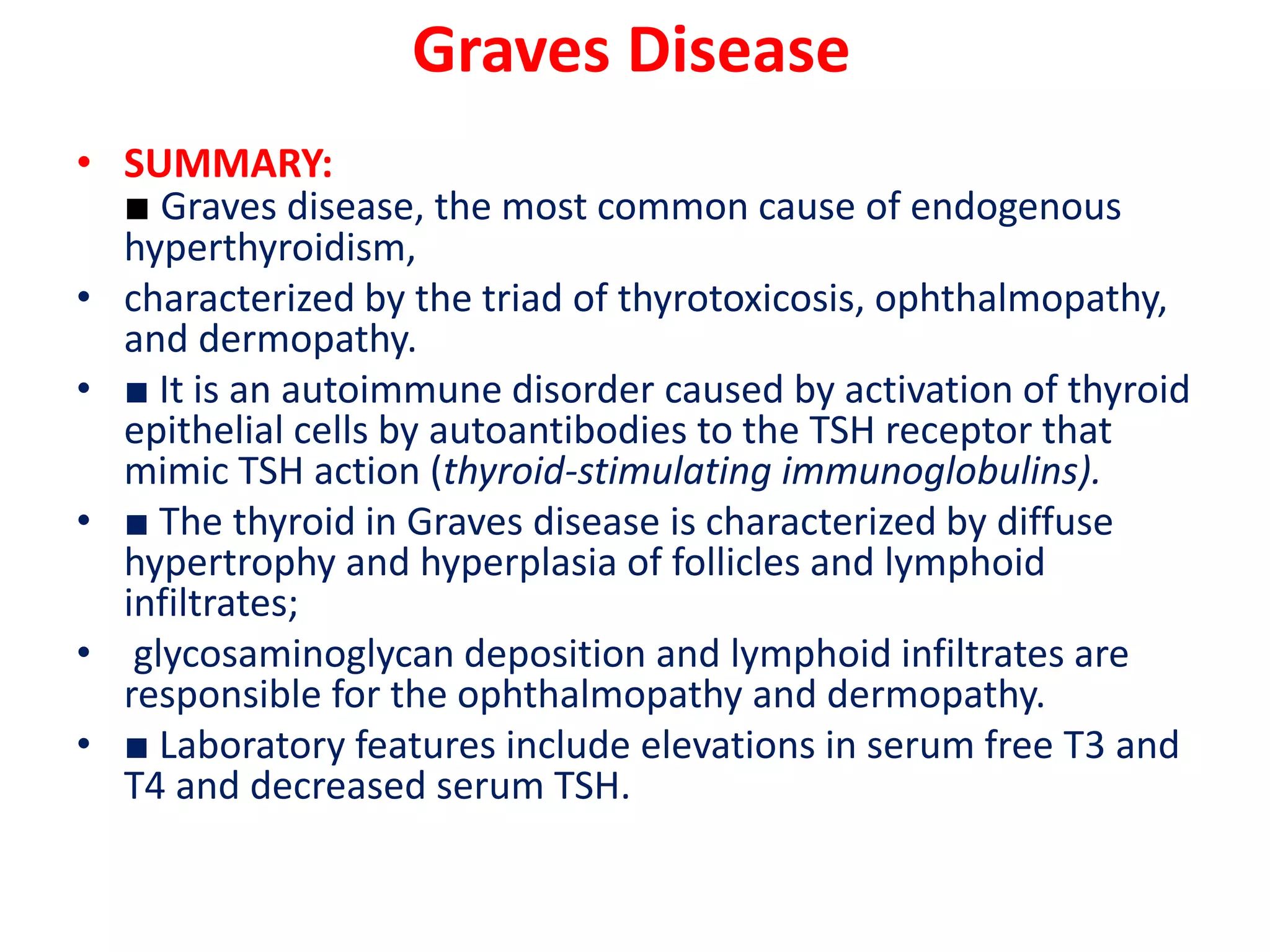
- Graves' disease is the most common cause of hyperthyroidism. It is characterized by the triad of thyrotoxicosis, ophthalmopathy, and dermopathy due to autoantibodies that mimic TSH.
- Hypothyroidism is most commonly caused by Hashimoto's thyroiditis, an autoimmune disorder characterized by lymphocytic infiltration and antibody production. Clinical manifestations range from mild to