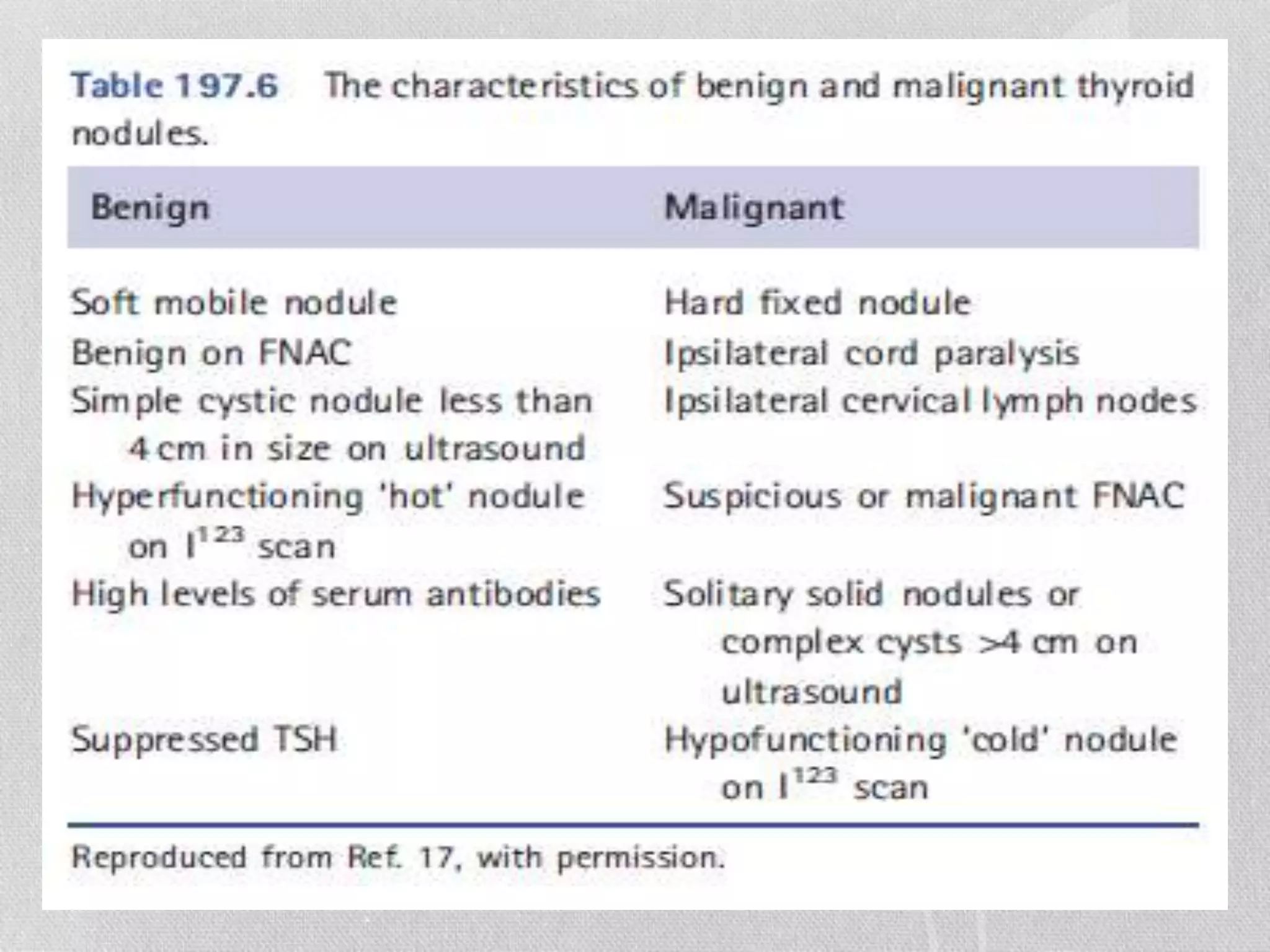
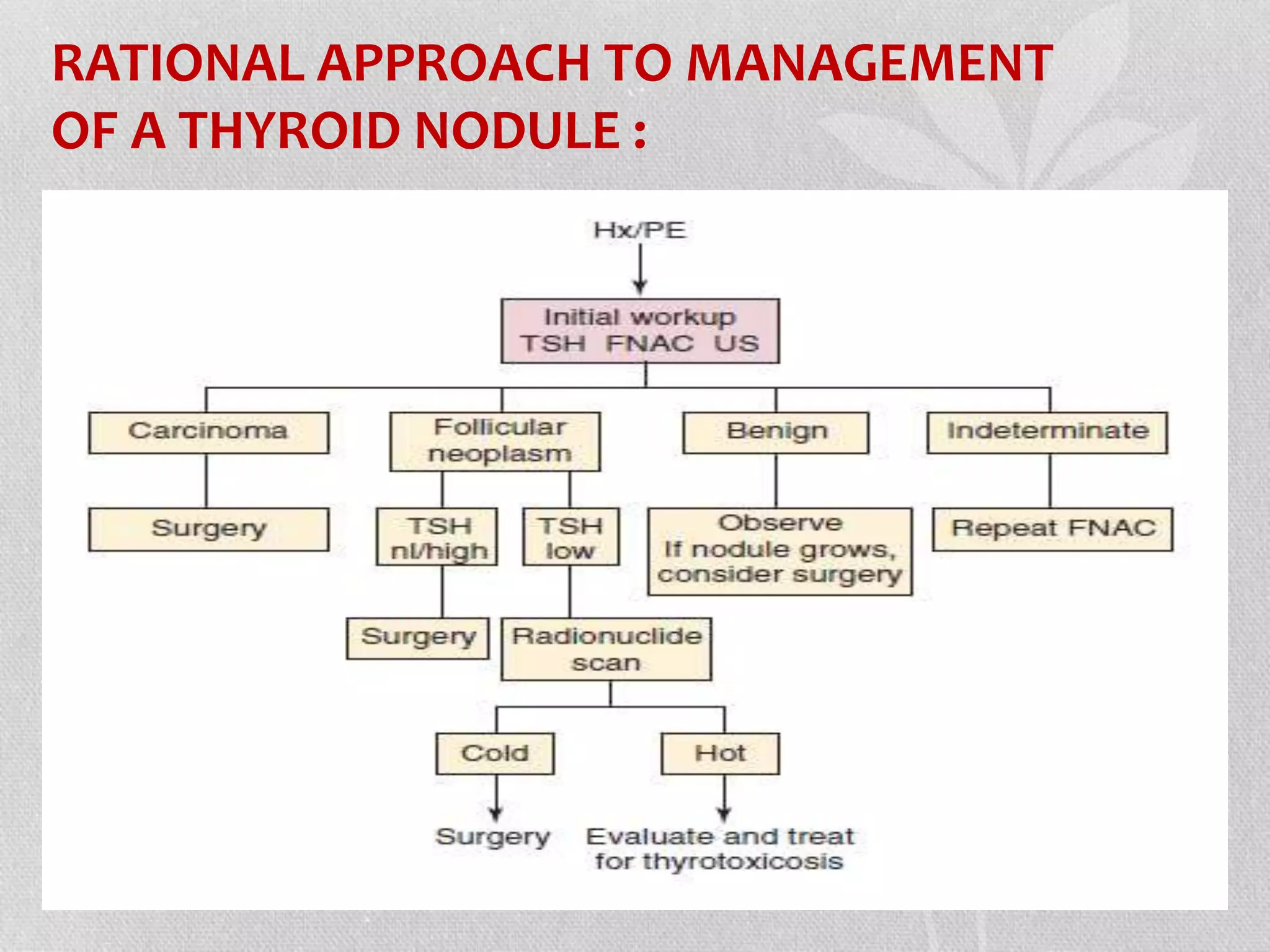
1) Thyroid nodules are common findings that require evaluation to determine if they are malignant or benign.
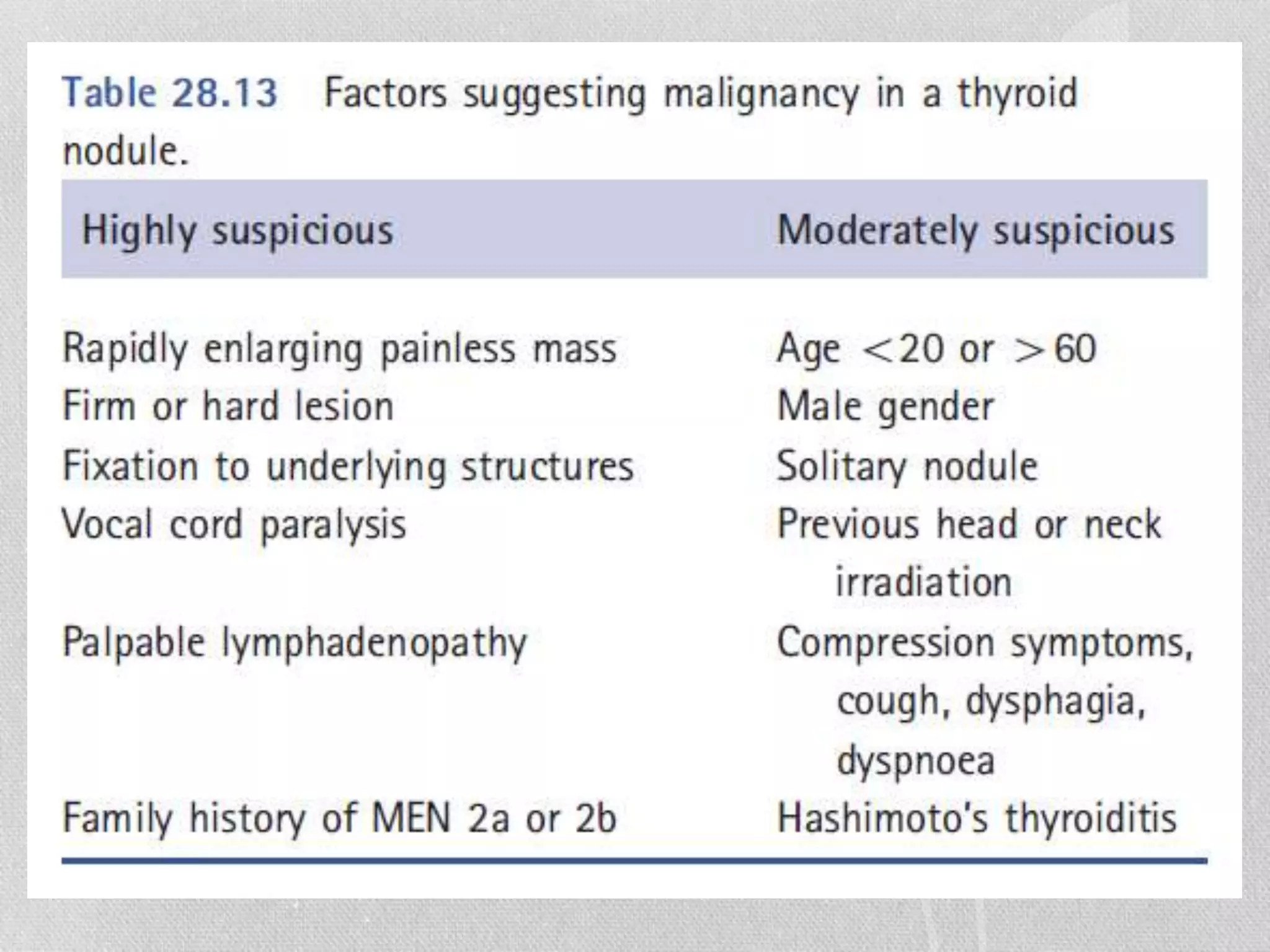
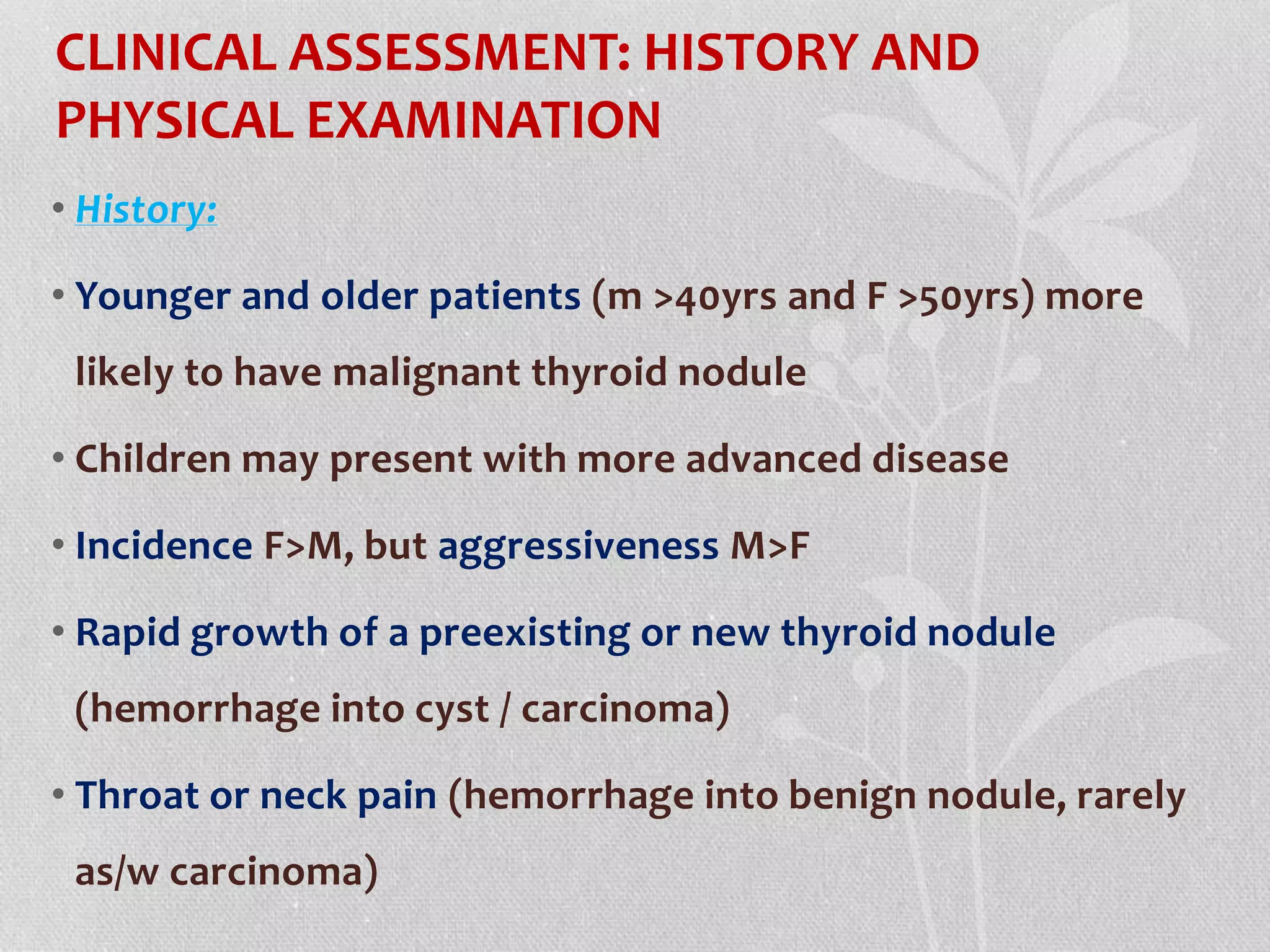
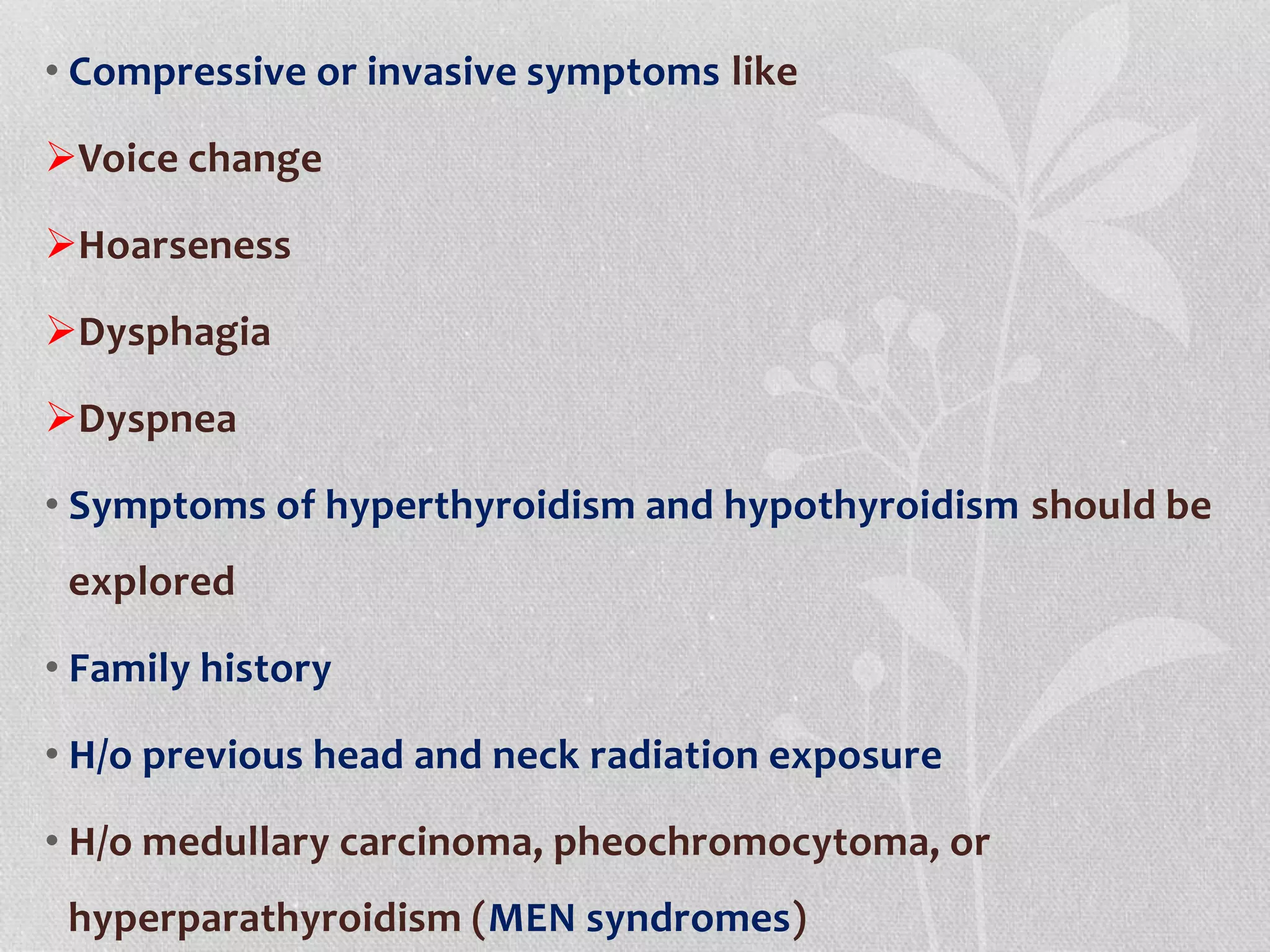
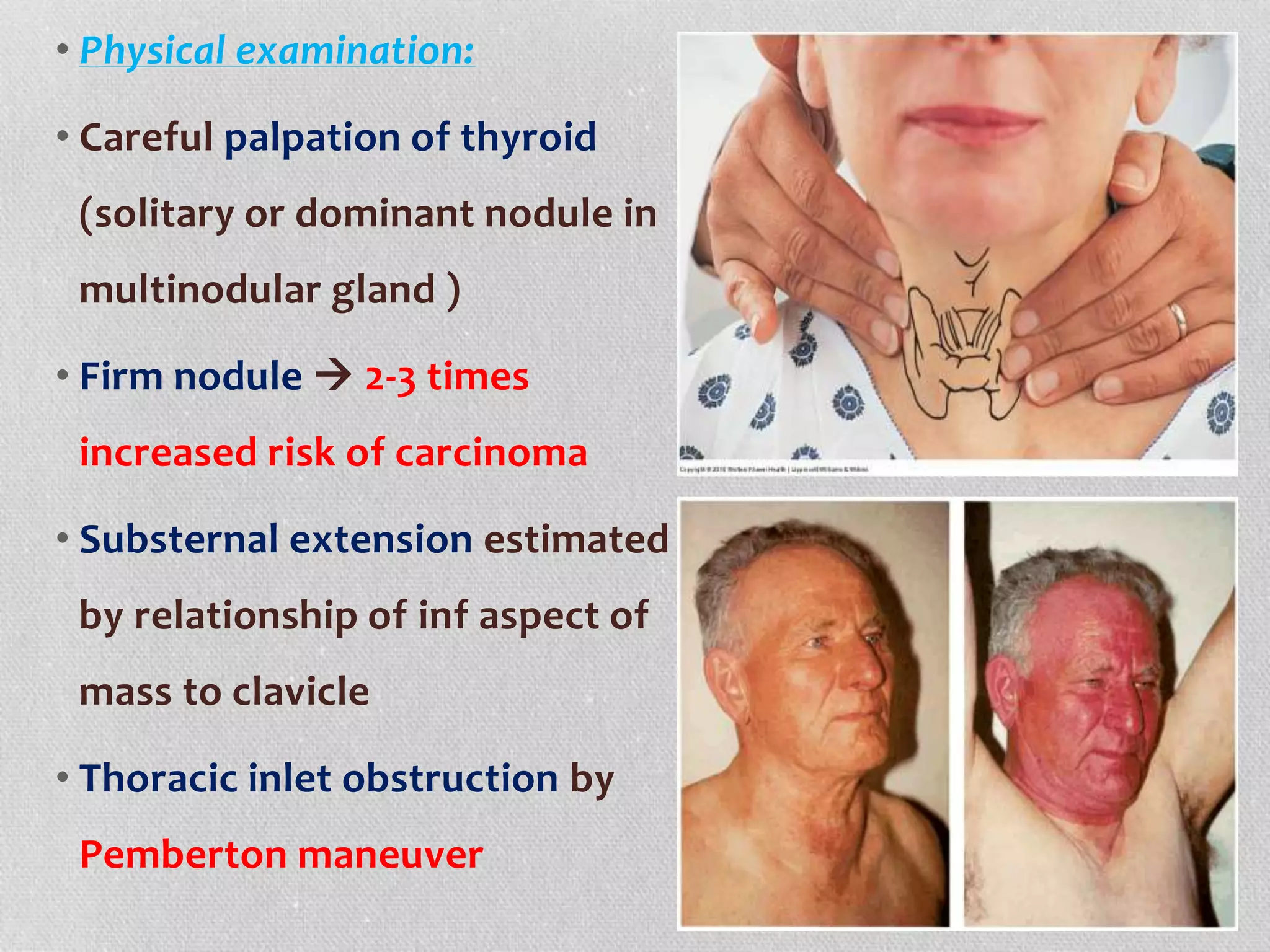
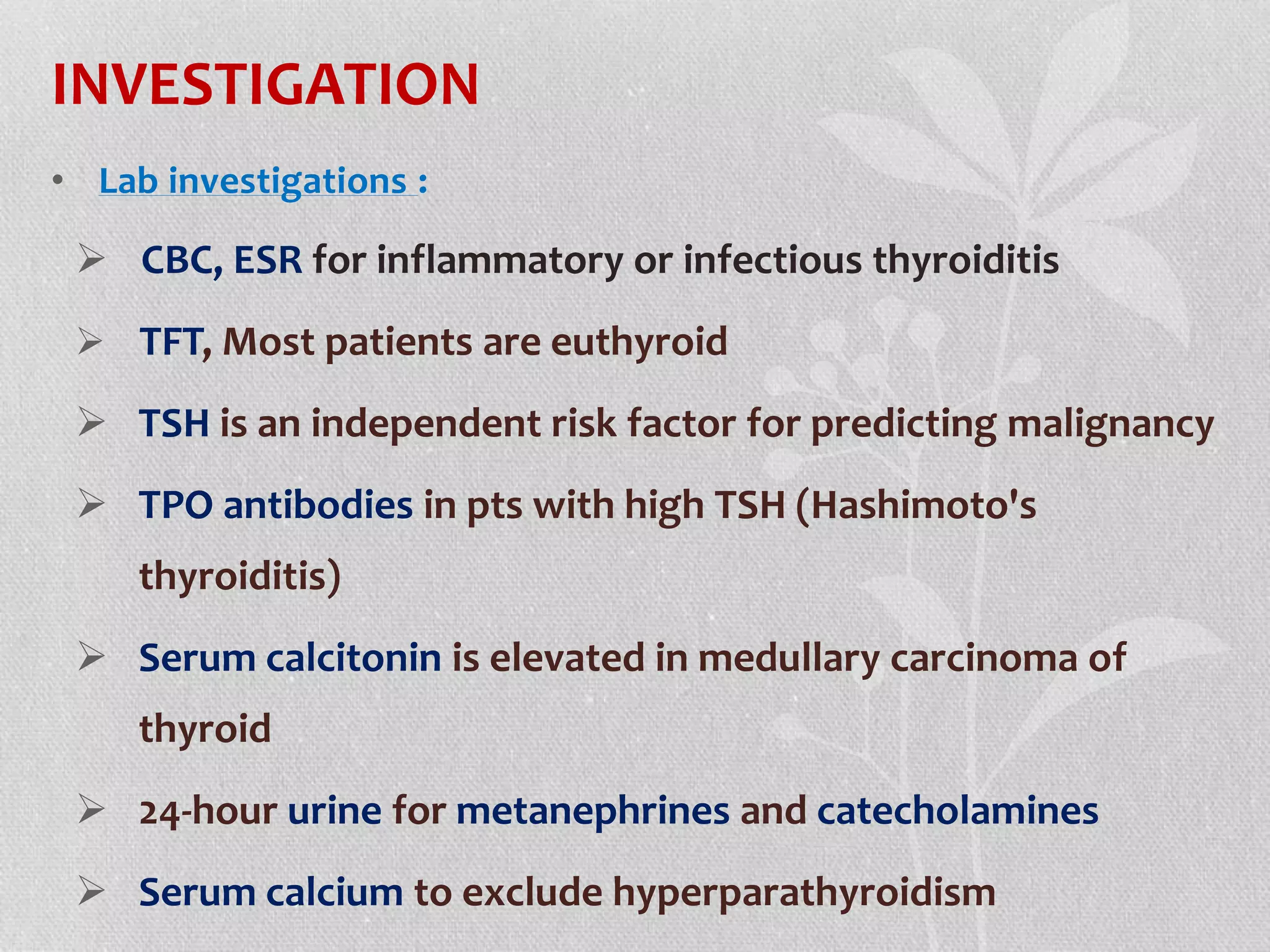
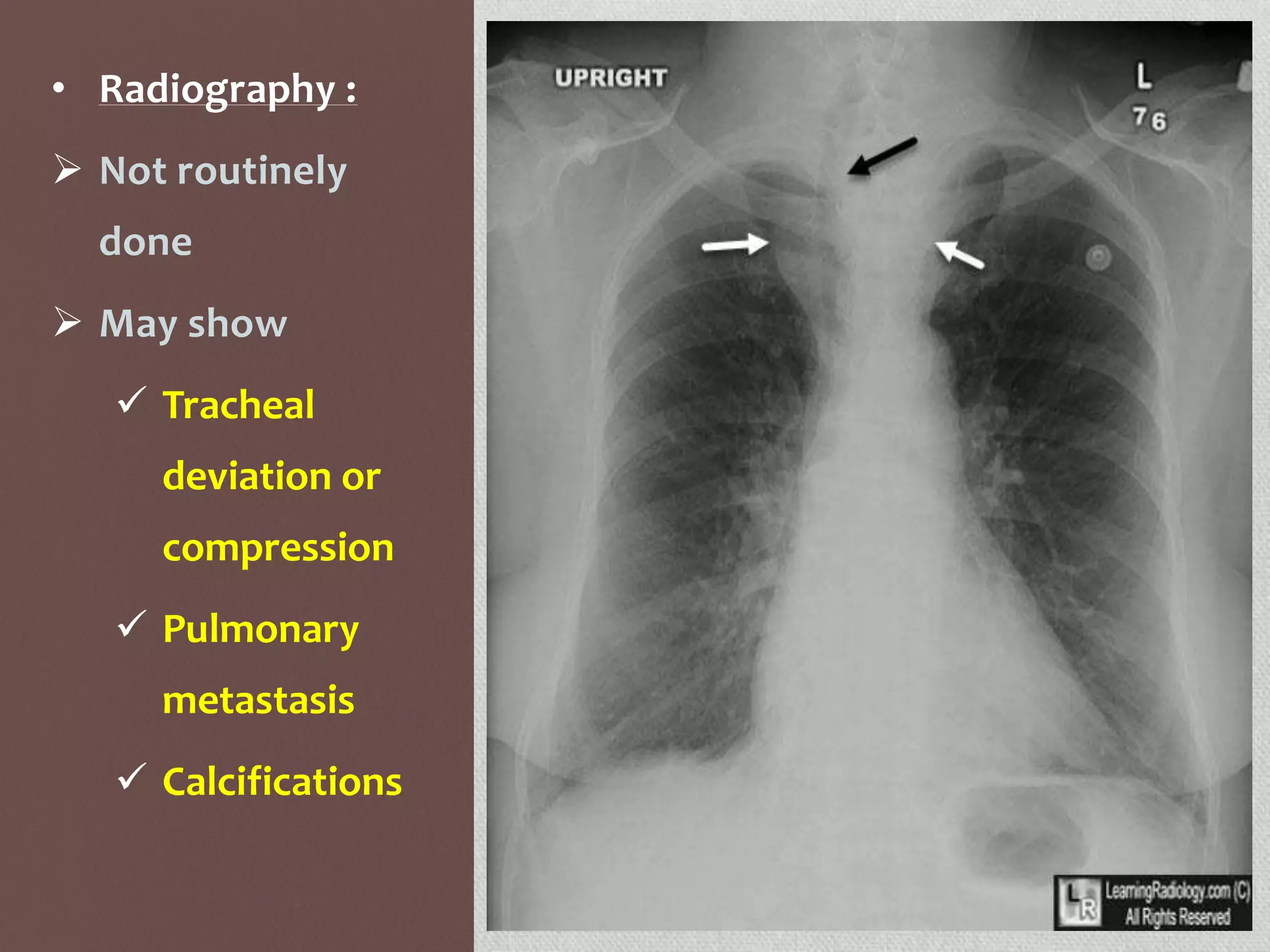
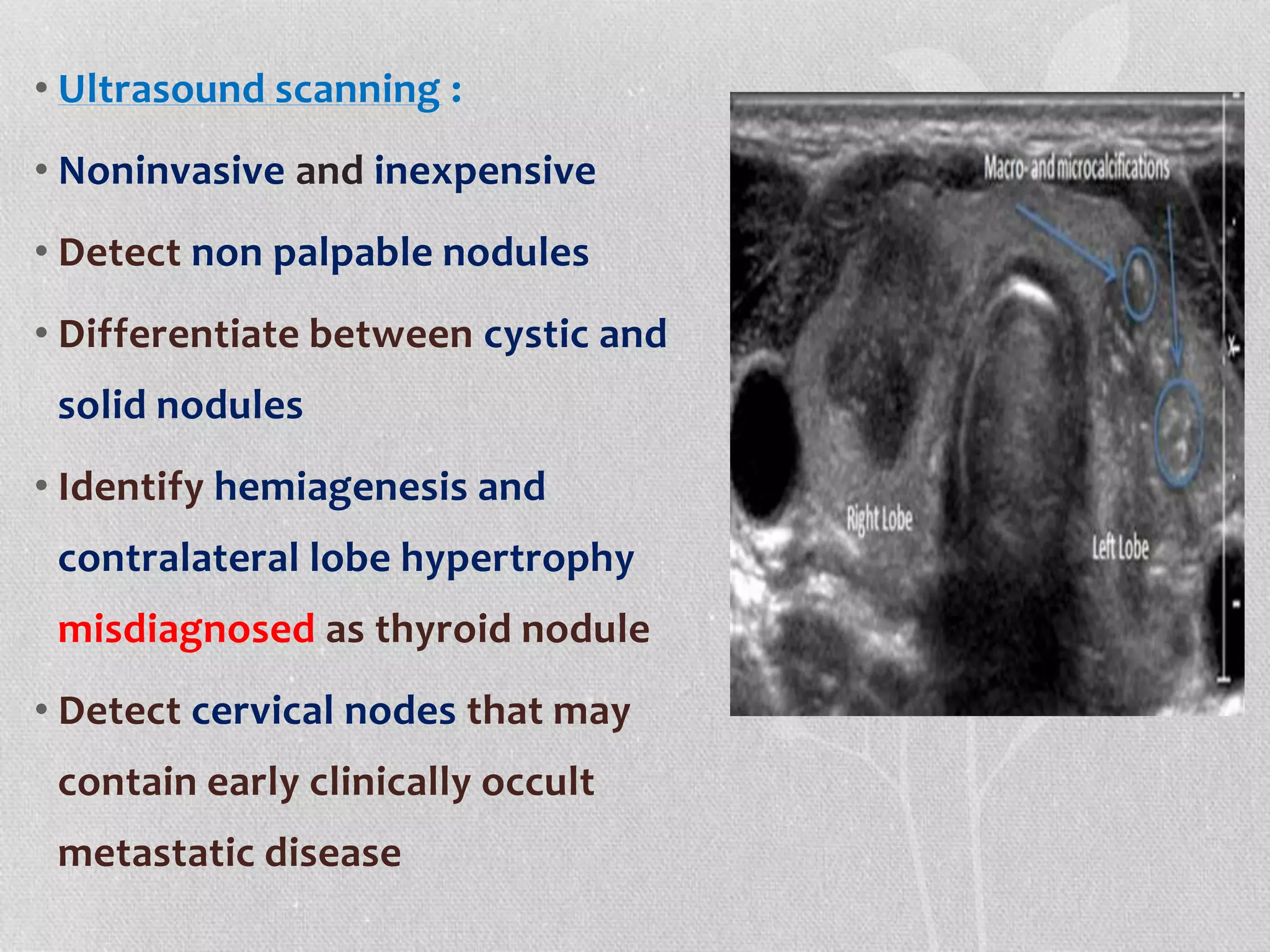
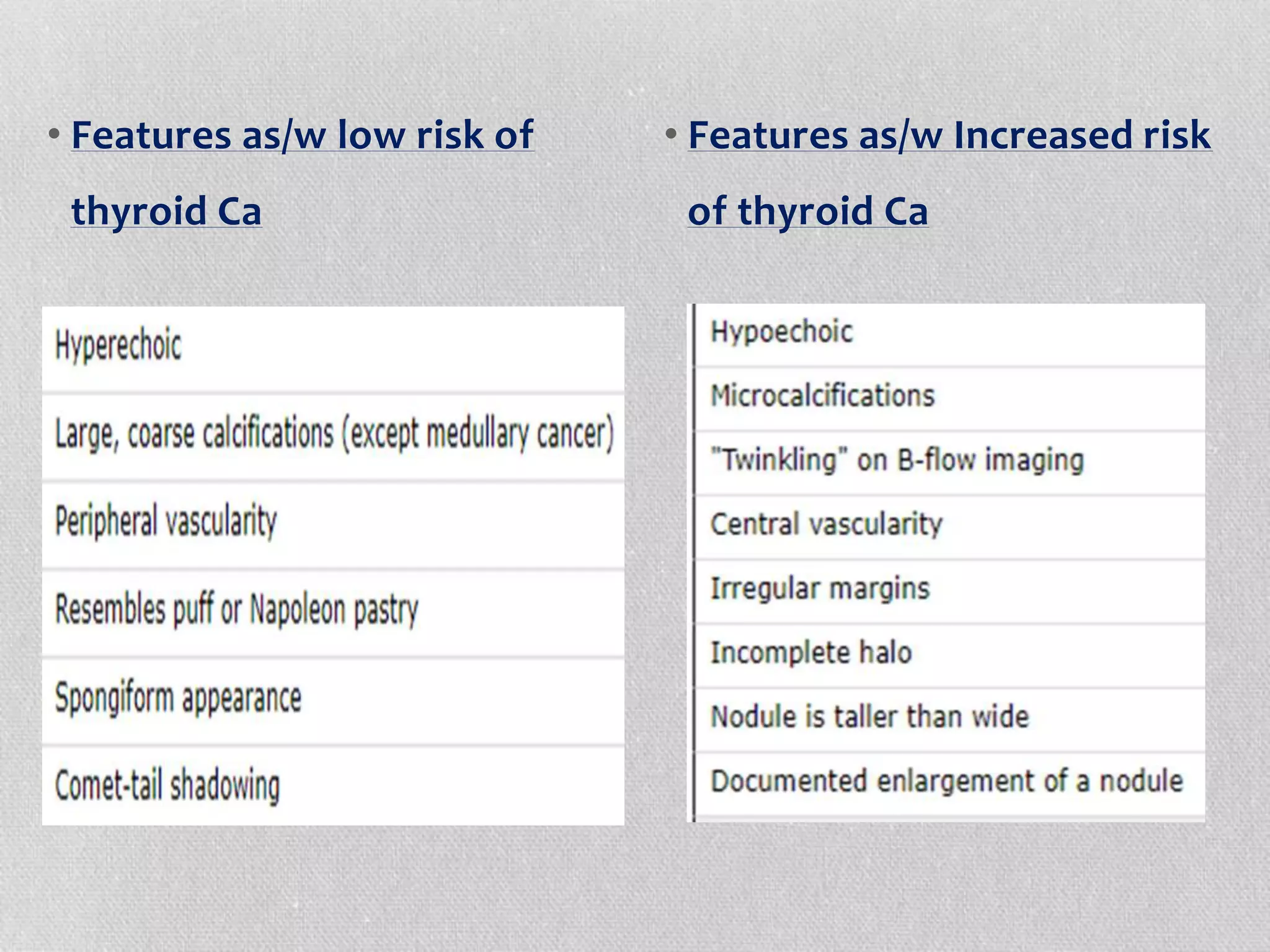
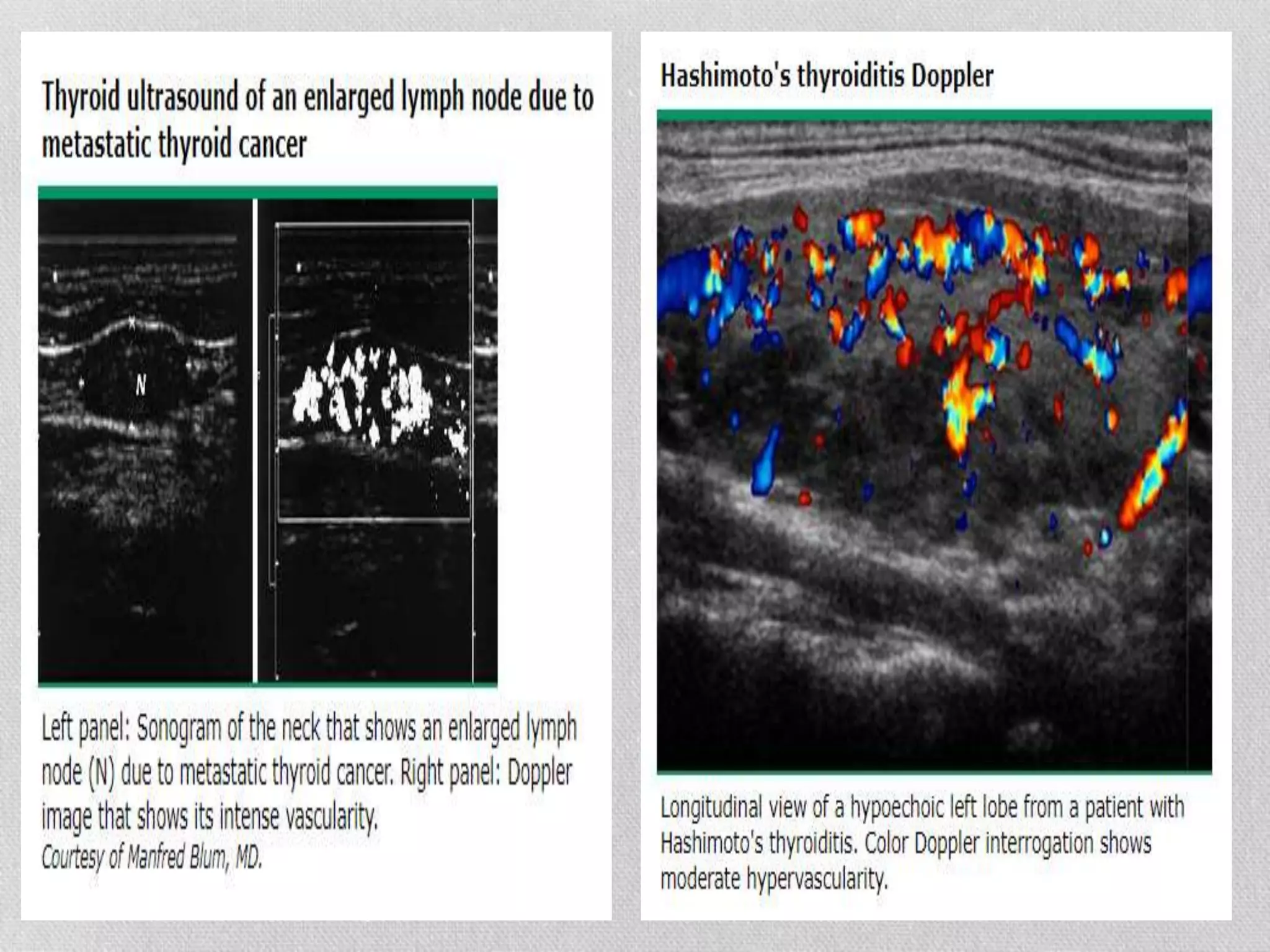
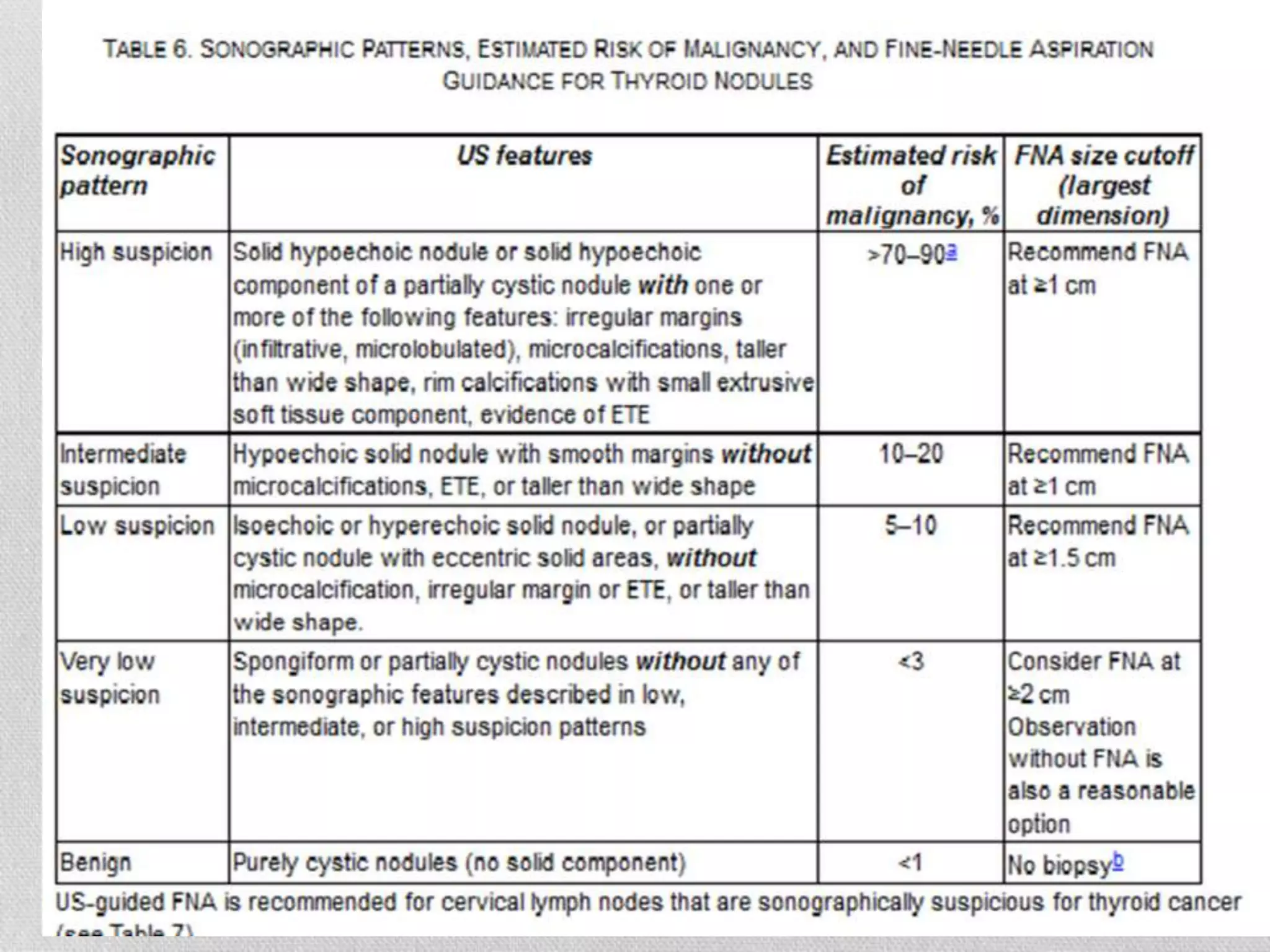
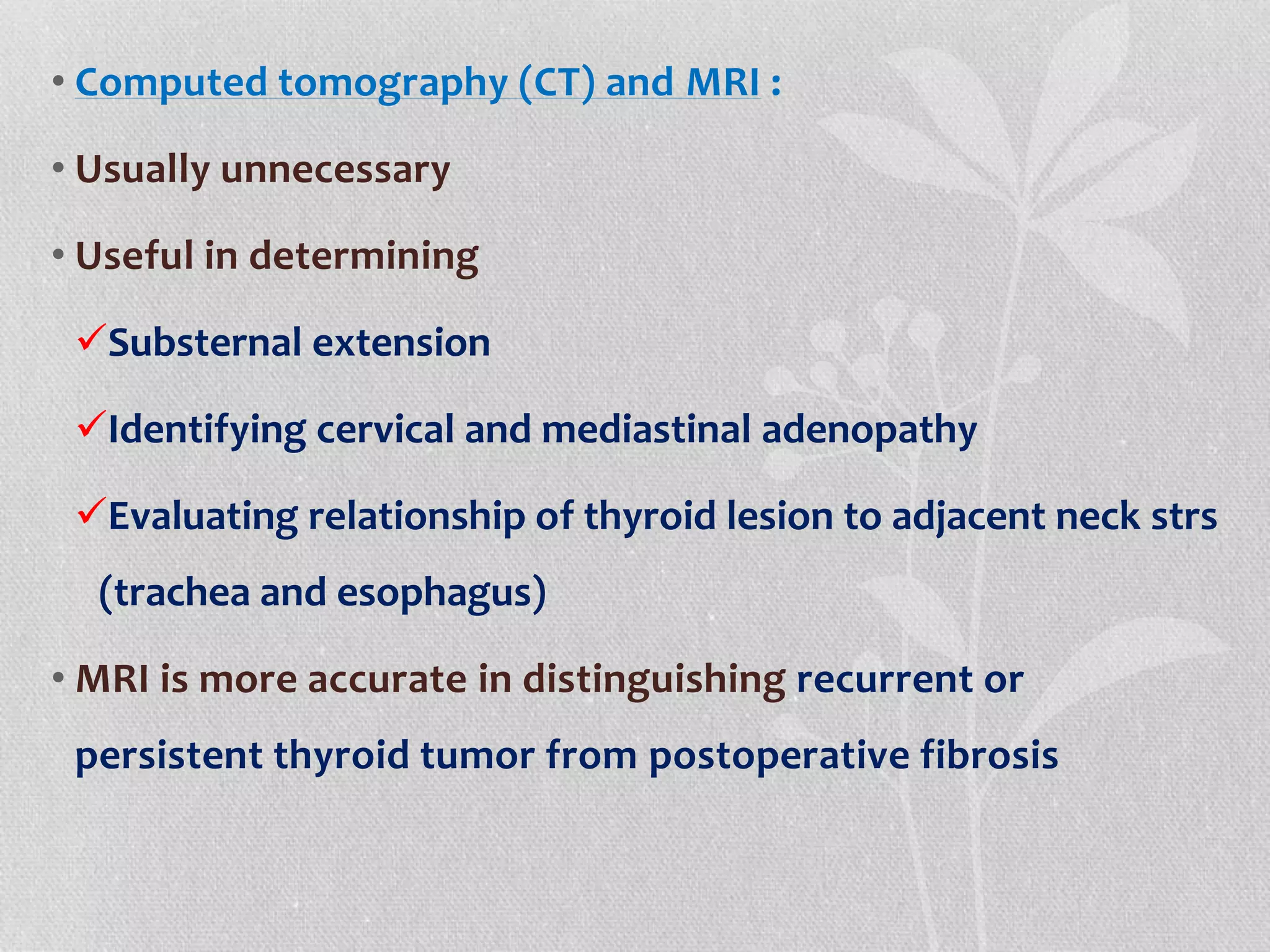
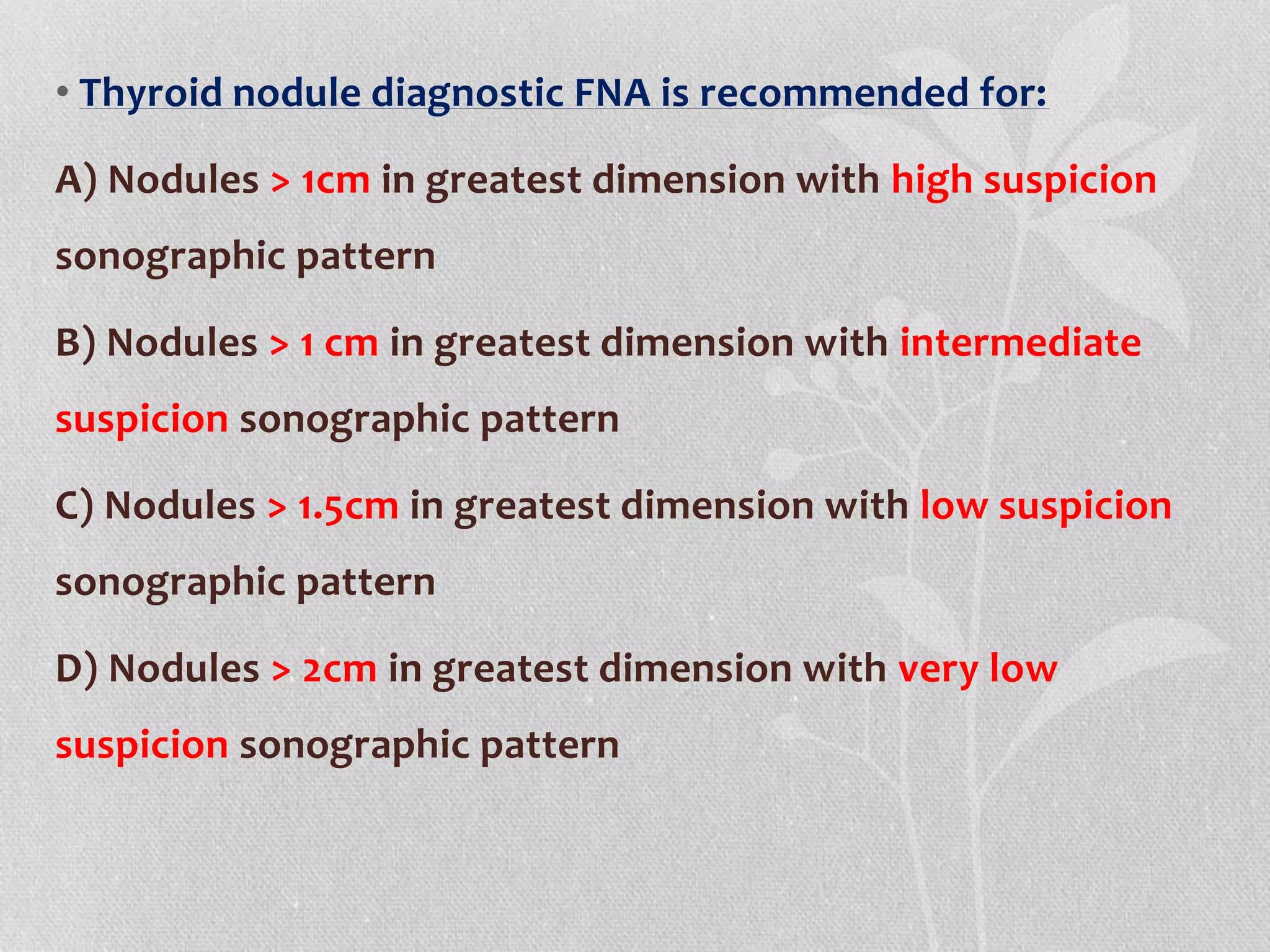
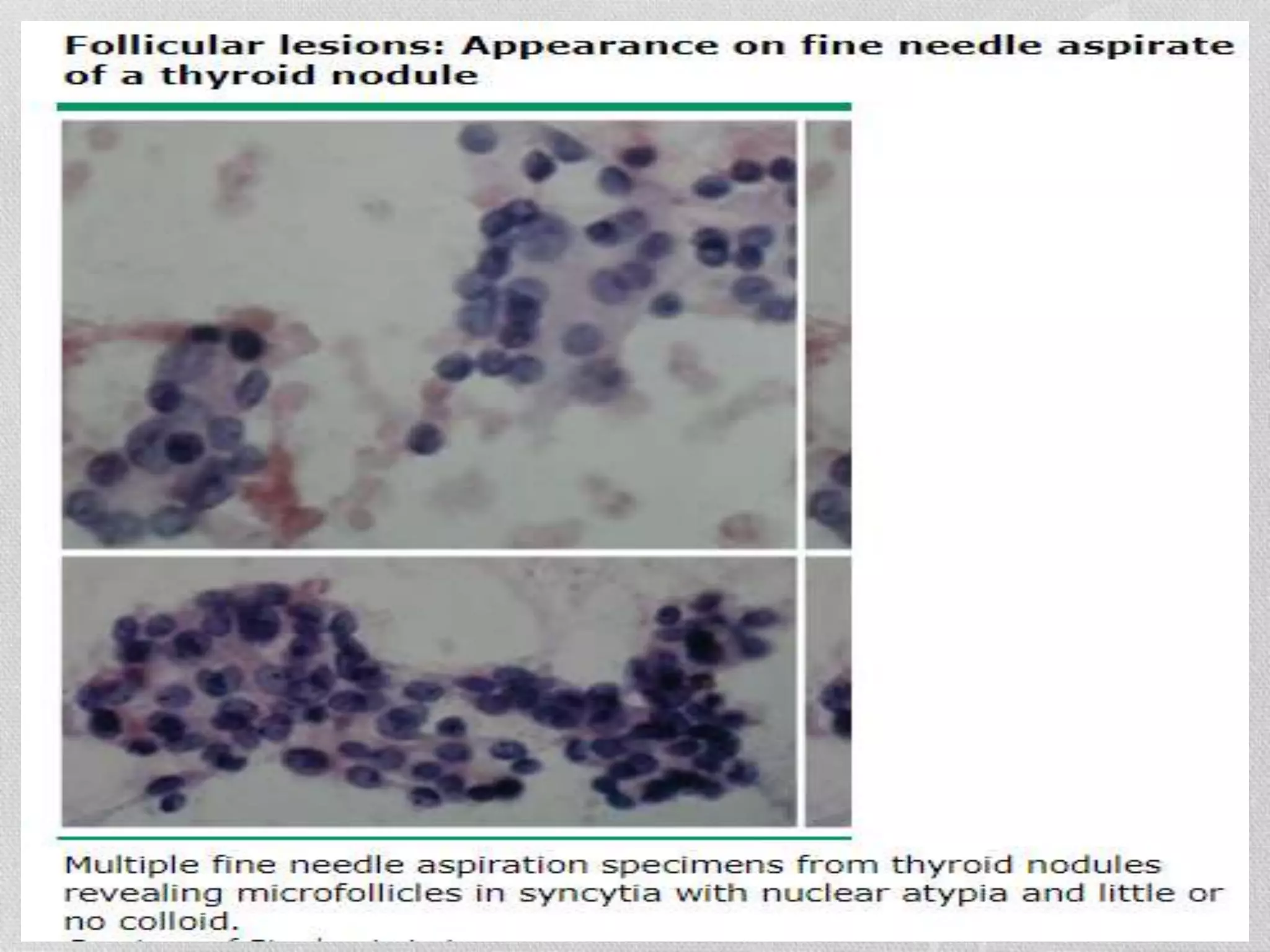
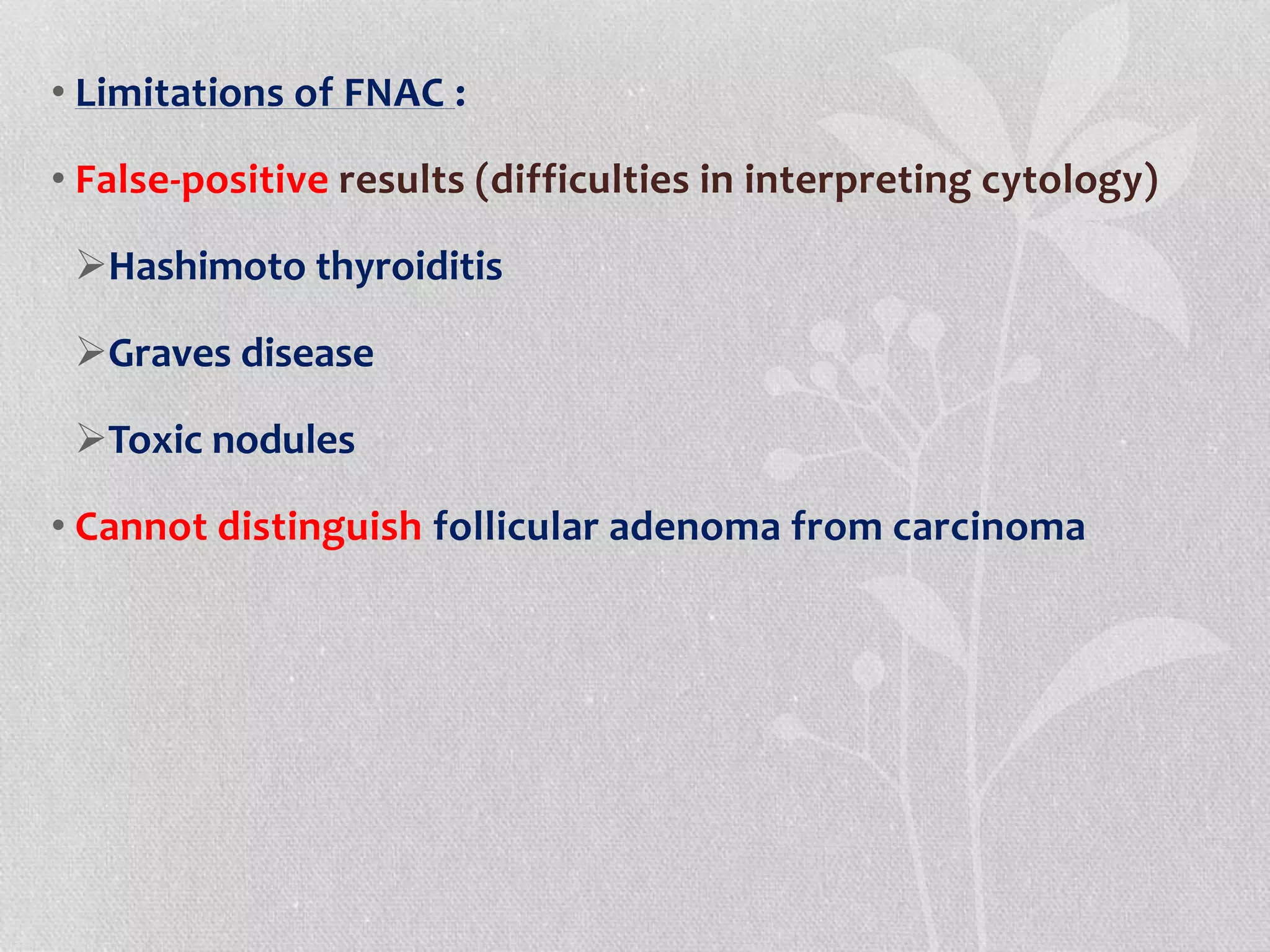
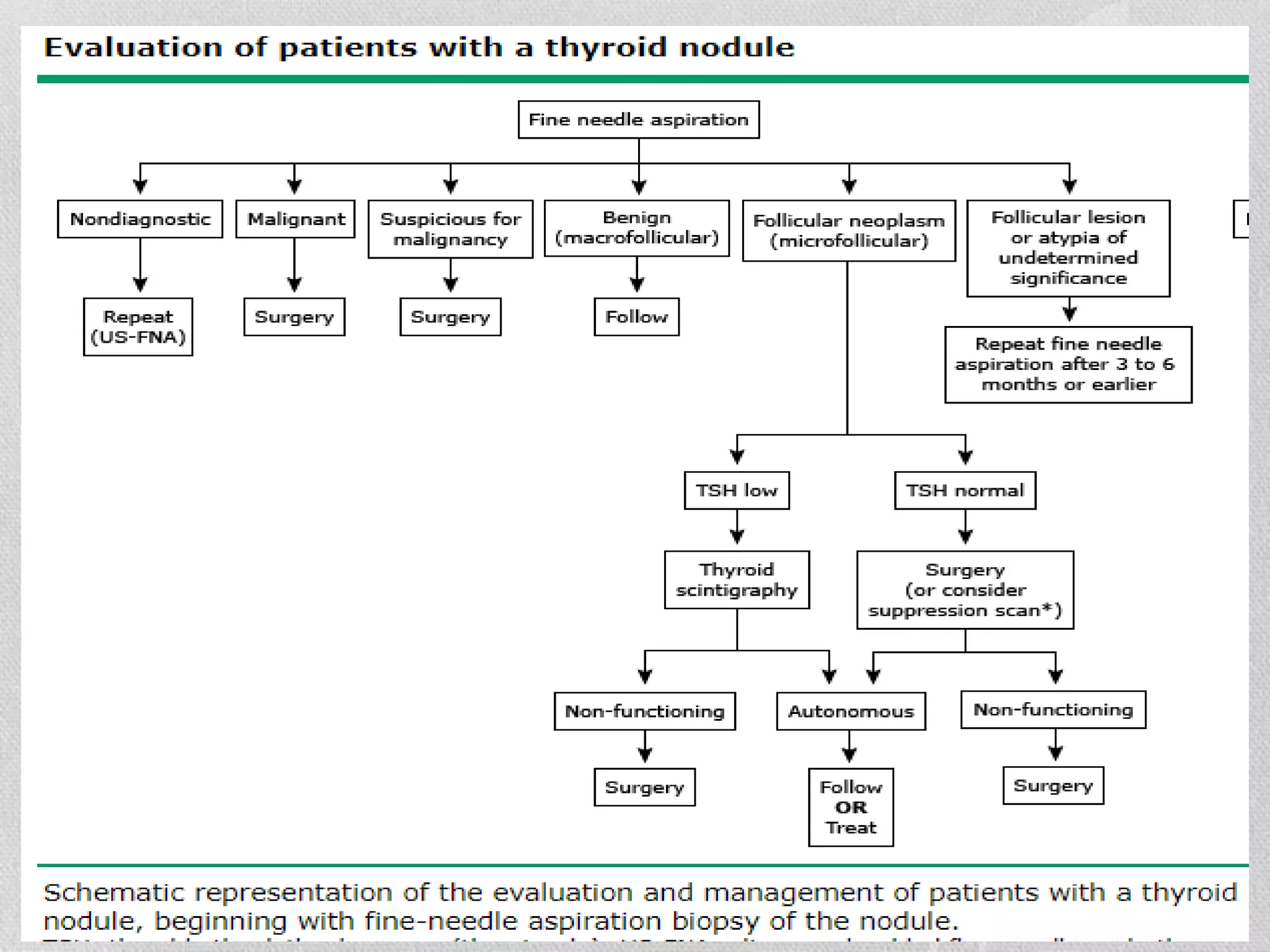
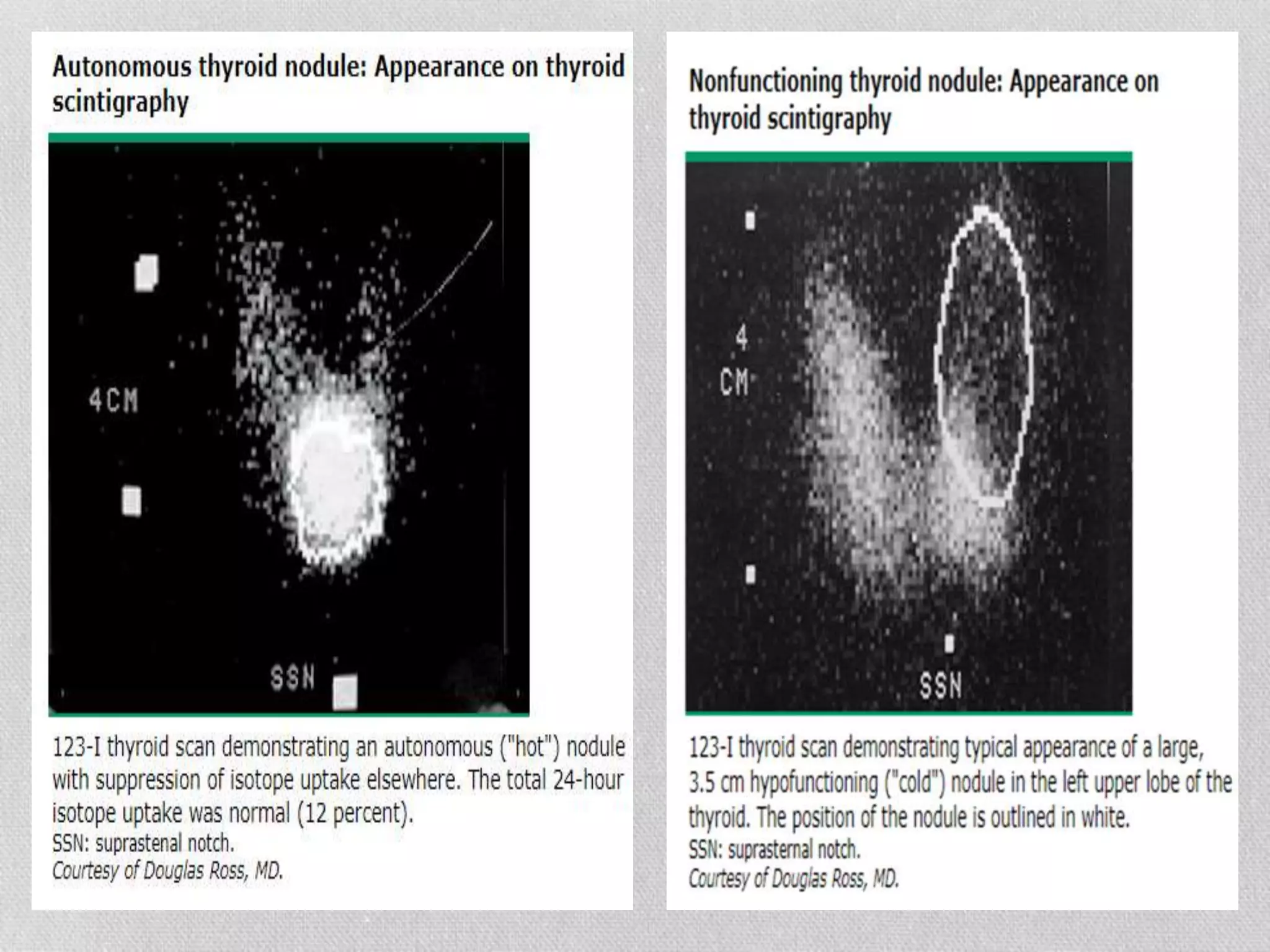
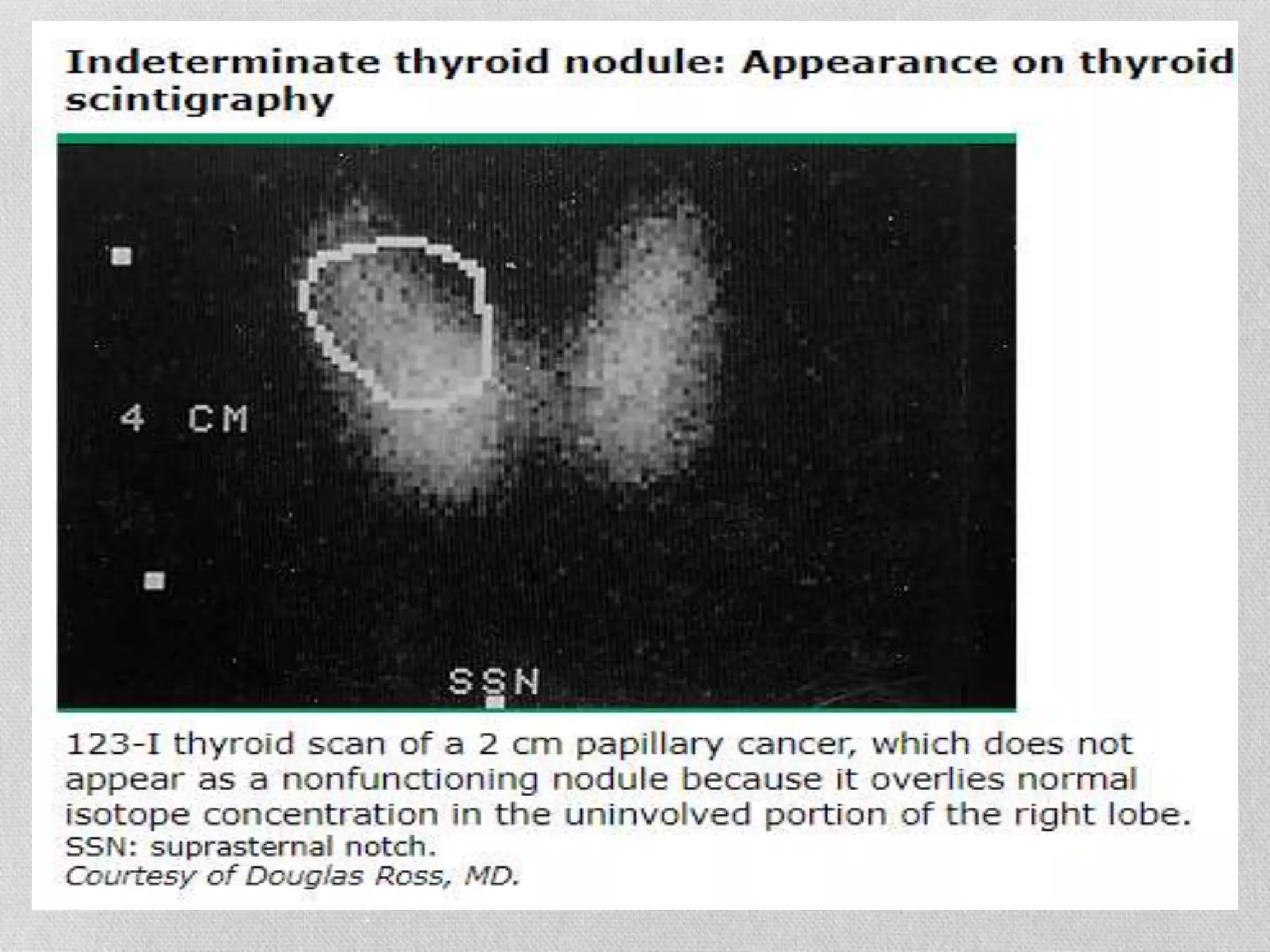
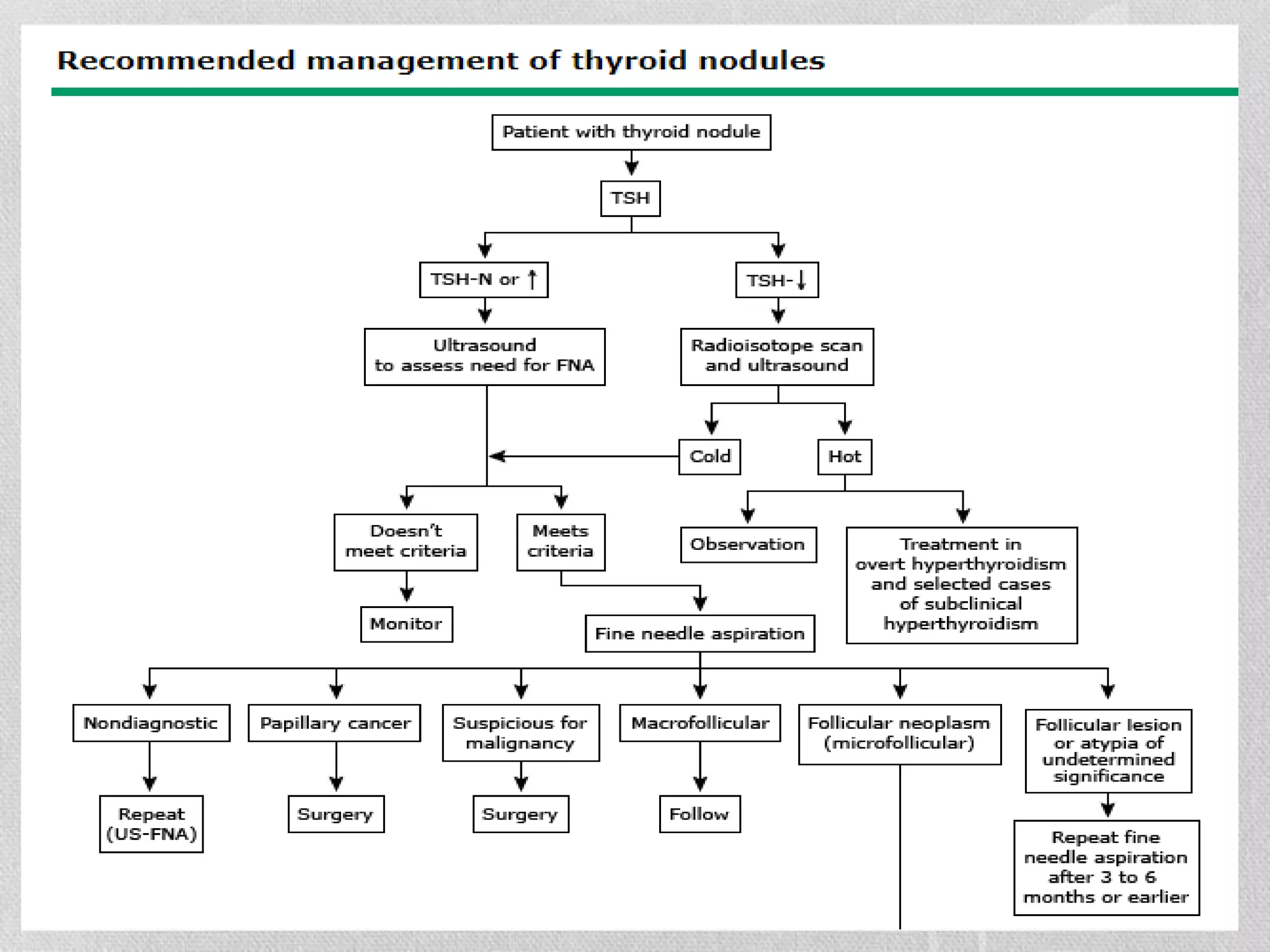
2) Evaluation involves patient history, physical exam, laboratory tests like TSH, ultrasound of the thyroid, and fine needle aspiration biopsy of suspicious nodules.
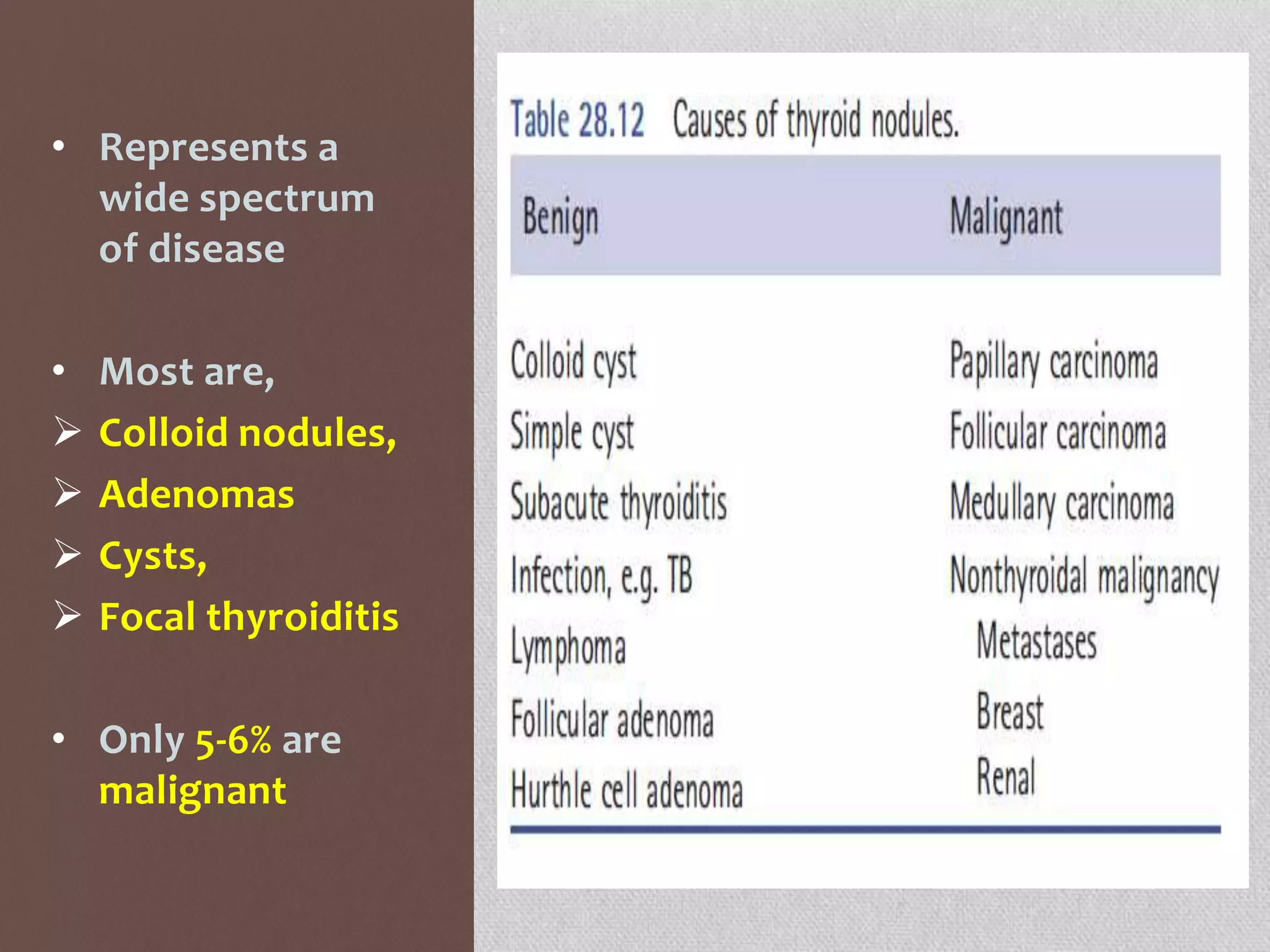
3) Most nodules are benign but ultrasound and biopsy help determine the small percentage that require surgical removal due to cancer risk.