Lung cancer remains a leading cause of cancer death. While early detection improves survival rates, past screening studies using chest x-rays and sputum analysis failed to reduce mortality. New screening methods using low-dose CT scans have shown promise in detecting early-stage cancers. However, limitations include high false positive rates and the need for improved methods to assess growth of small nodules over time. Further research is still needed to determine if lung cancer screening using low-dose CT can reduce mortality and be cost-effective.
![Lung cancer remains the leading cause of mortality from
cancer. In 1999, there were approximately 170,000 new
cases of lung cancer [1].
The 5-year survival rate from the disease is 14% and has
increased only slightly since the early 1970s despite an
extensive and costly research effort to find effective
therapy.
1. Landis SH, Murray T, Bolden S, Wingo PA. Cancer
statistics, 1999. Cancer J Clin 1999; 49:8–31.](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-3-320.jpg)
![The disparity in survival between early- and late-stage
lung cancer is substantial, with a 5-year survival rate of
approximately 70% in stage 1A disease compared to less
than 5% in stage IV disease according to the recently
revised Lung Cancer Staging criteria [2]. Unfortunately, as
many as 60% of patients present with advanced-stage
lung cancer.
2. Mountain CF. Revisions in the international system for
staging lung cancer. Chest: 1997:111:1710-1717
.](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-4-320.jpg)
![The disproportionately high prevalence and mortality of
advanced lung cancer has encouraged attempts to
detect early lung cancer with screeningprograms aimed
at smokers. Smokers have an incidence rate of lung
cancer that is 10 times that of nonsmokers and account
for greater than 80% of lung cancer cases in the United
States [3]. Until recently, two main approaches have
been used to screen for lung cancer: chest radiography
and sputum cytology](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-5-320.jpg)
![Two other studies have been reported from Europe that
assessed the screening potential of chest radiography
for lung cancer . A randomized controlled study from
Czechoslovakia reported in the mid-1980s evaluated
6364 male smokers between the ages of 40 and 64
[9,10]. Both screened and control groups were followed
over a 3-year period. The screened group (n 3172)
underwent both a chest radiograph and sputum
cytology every 6 months for the duration of the study.
The control group (n 3174) received only a chest
radiograph at the end of the 3-year period. Thirty-nine
cancers were detected in the screened group compared
to 27 in the control group. However, no clear advantage
in mortality was demonstrated in the screened group.](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-11-320.jpg)
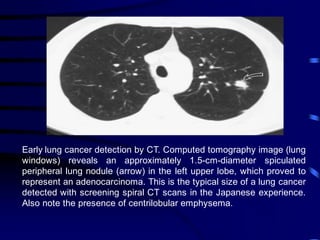
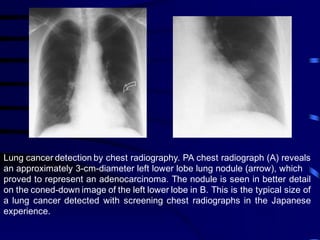
![In 1996, Kaneko et al. reported the use of biannual chest
radiographs and spiral CT scans in screening 1369
Japanese adults at high risk for developing lung cancer
[18]. Peripheral lung cancer was detected in 15 (1%)
subjects by CT but in only 4 (0.3%) by chest radiography. A
vast majority (93%) of detected cancers was classified as
Stage I.](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-14-320.jpg)
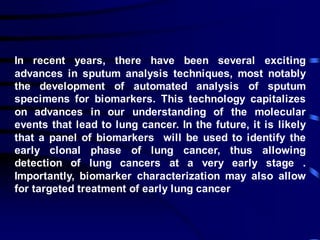
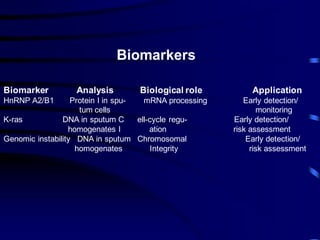
![C. Sputum Cytology and Advanced Sputum
Analysis Techniques:
In screening studies, the sensitivity of sputum
cytology for detecting lung cancer is approximately 20
to 30% and the specificity is approximately 98%
.Improvement in sensitivity can be achieved by
adherence to proper techniques for collection,
processing, and interpretation of samples [48].
Sputum cytology demonstrates the highest sensitivity
for squamous cell carcinoma and the lowest yield for
adenocarcinoma .](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-35-320.jpg)
![Because of its invasive nature and high cost,
screening with AF should currently be reserved for
patients with a very high pretest probability of lung
cancer .For widespread screening, AF should ideally
be coupled with a noninvasive, first-line study that
selects patients with a high pretest probability of
harboring early lung cancer .For example, a recent
study by Phillips et al. describes the use of a
breathalyzer to identify volatile organic compounds
that may serve as potential markers for lung cancer
[61]. Future studies are needed to determine the
precise role of this exciting new technology in the
detection of early lung cancer.](https://image.slidesharecdn.com/lungcancerscreening-161107104729/85/Lung-Cancer-Screening-41-320.jpg)