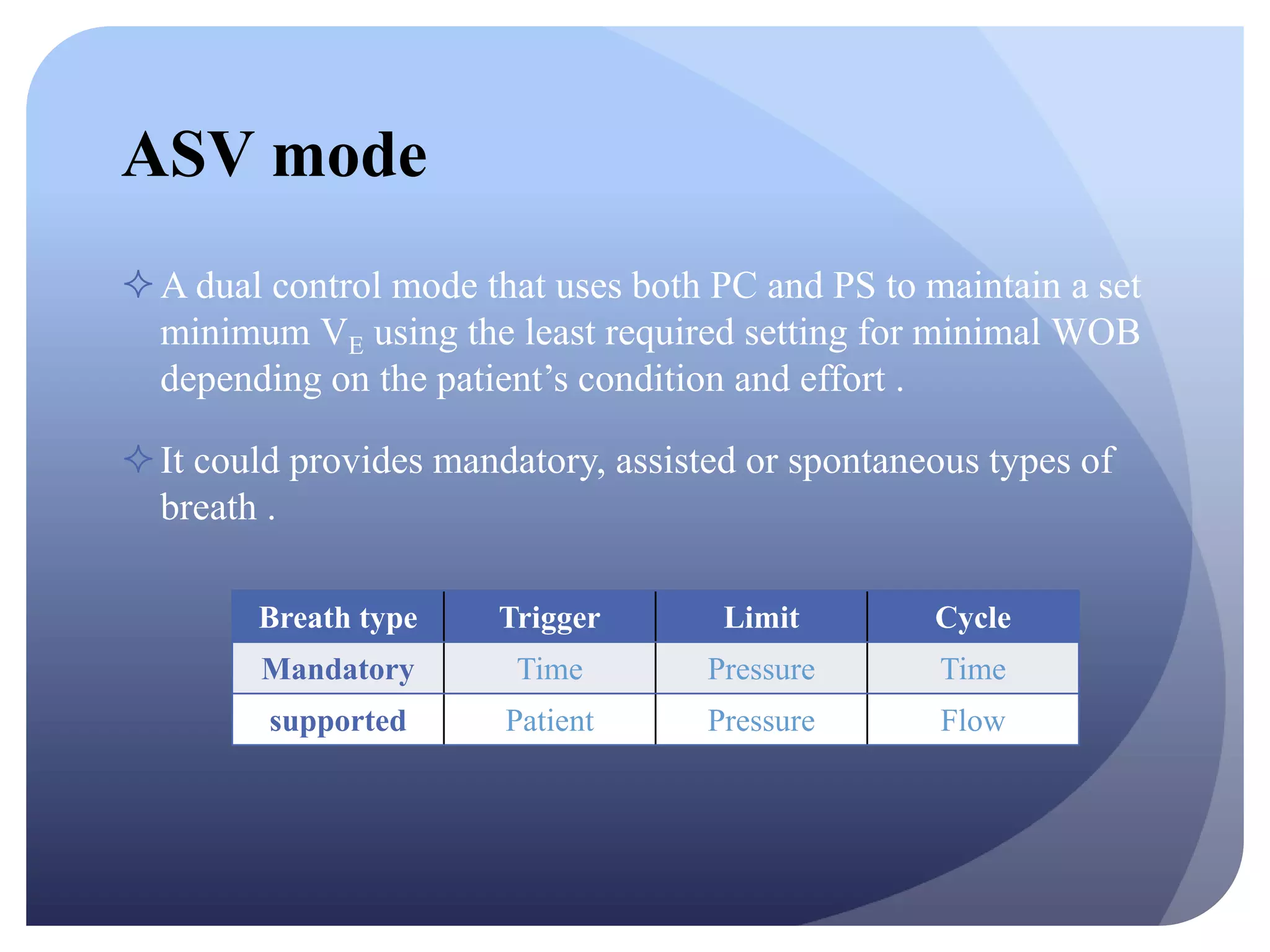
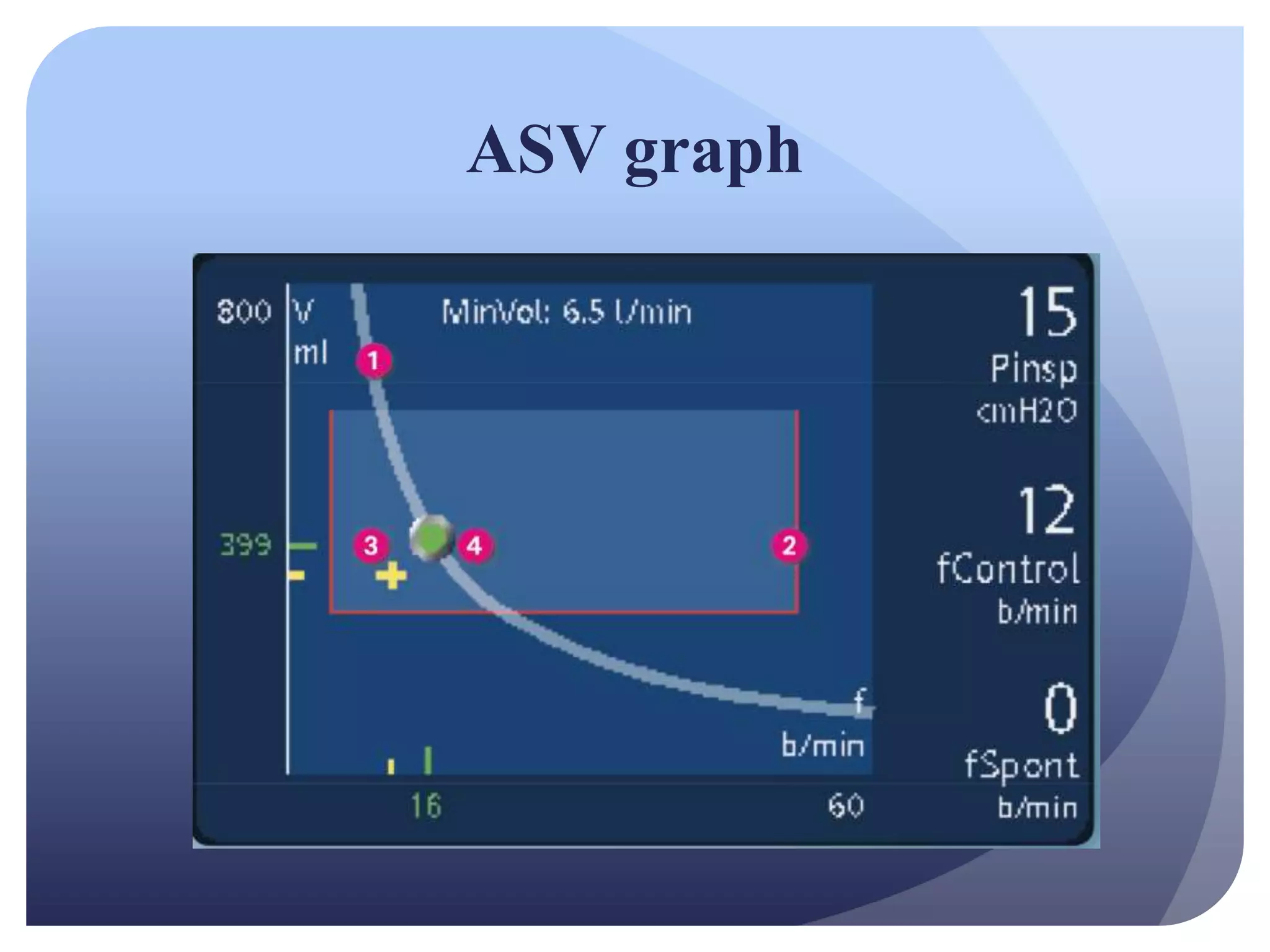
Adaptive Support Ventilation (ASV) is a specialized ventilation mode designed for intubated patients, providing a combination of pressure-controlled and volume-targeted support to optimize patient outcomes. It automatically adjusts to patient needs, requiring minimal user intervention while promoting weaning and reducing ventilation times. The mode's safety and effectiveness have made it a preferred choice for managing diverse patient groups, including those with COPD and ARDS.