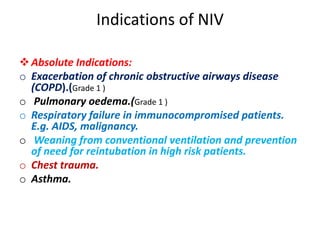
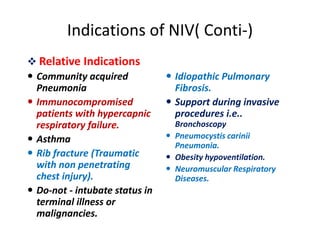
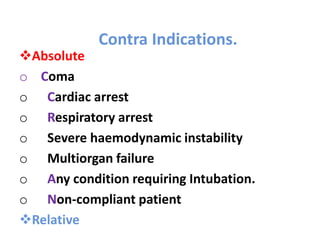
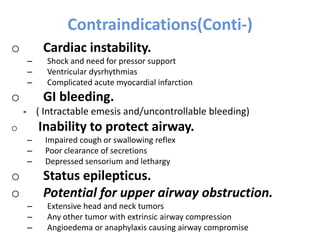
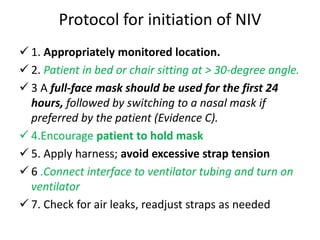
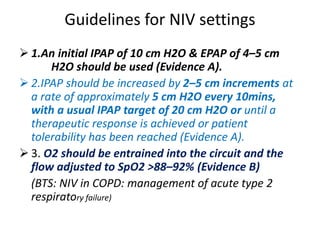
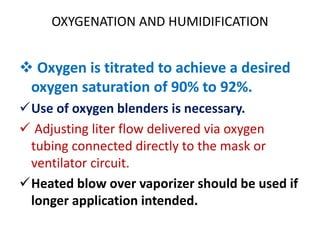
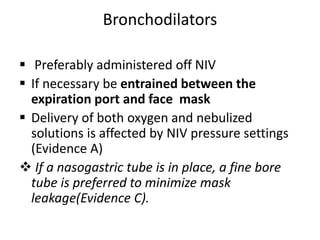
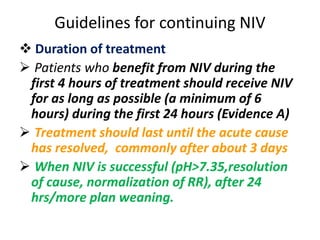
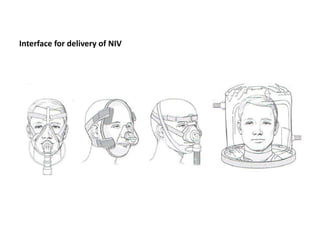
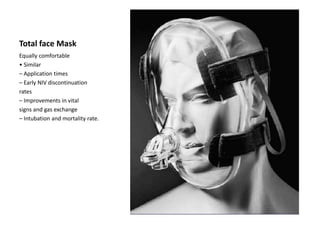
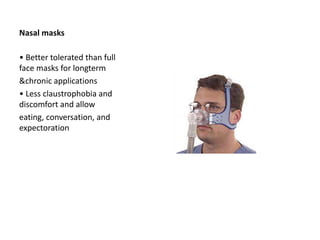
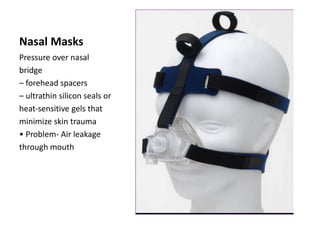
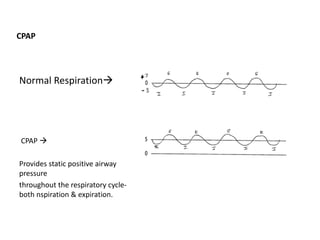
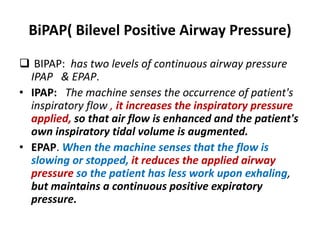
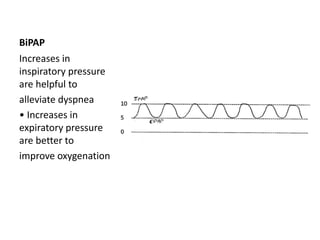
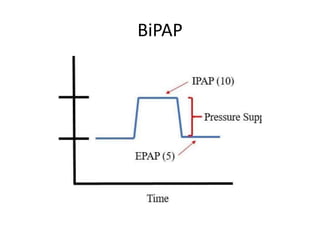
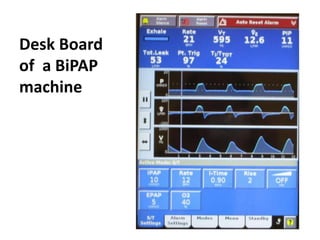
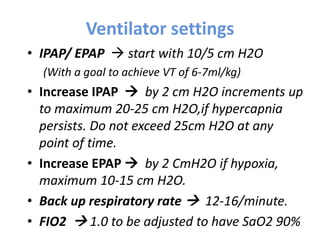
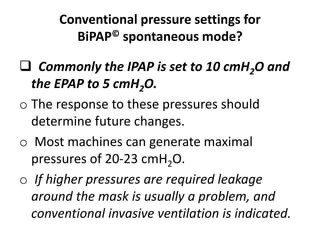
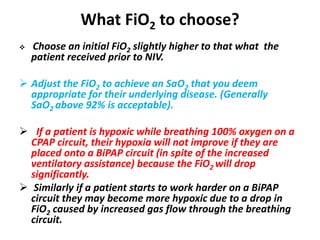
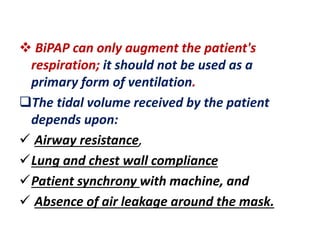
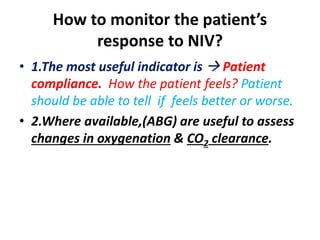
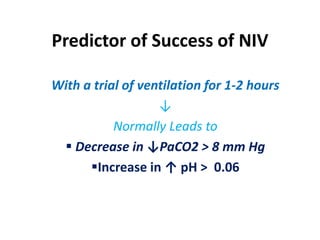
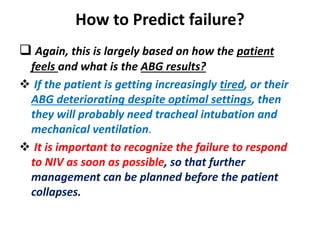
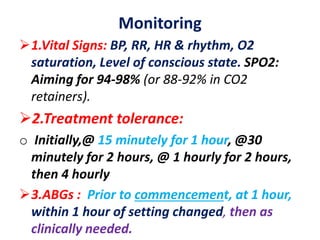
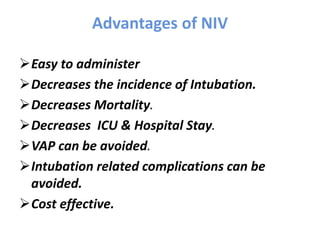
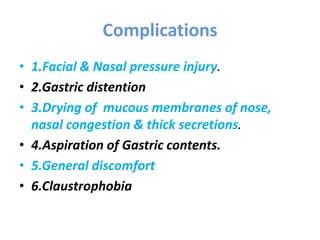
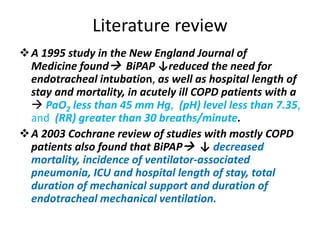
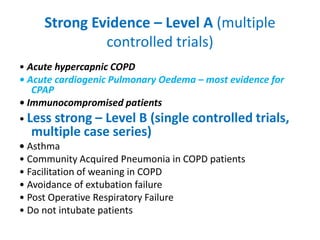
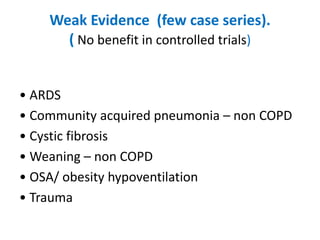
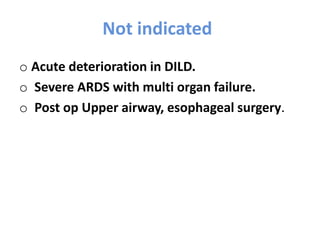
Non Invasive Ventilation (NIV) involves delivering mechanical ventilation without the use of an endotracheal tube or surgical airway, instead using a tight-fitting face or nasal mask. NIV has been used since the 1940s but became more widely used starting in the 1980s for conditions like sleep apnea. It is now commonly used to treat acute respiratory failure from COPD exacerbations and cardiogenic pulmonary edema. NIV can be delivered via CPAP or BiPAP and involves optimizing settings like IPAP, EPAP, respiratory rate and oxygen flow to improve ventilation and oxygenation without the need for intubation. Proper patient selection, interface choice, and monitoring are important for successful NIV treatment.