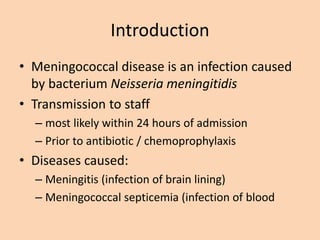
This document discusses Meningococcal disease, which is caused by the bacterium Neisseria meningitidis. It can cause meningitis (infection of the brain lining) or meningococcal septicemia (blood infection). The disease is transmitted through respiratory secretions. Specimens should be collected from patients for diagnosis. Morphologically, N. meningitidis appears as gram-negative oval or spherical diplococci. It grows on blood and chocolate agar. Antibiotic prophylaxis should be given within 24 hours to exposed individuals. Recommended antibiotics include rifampin, ciprofloxacin, or ceftriaxone. Health care workers caring for patients must take precautions