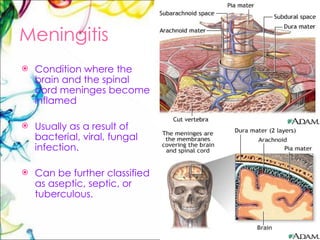
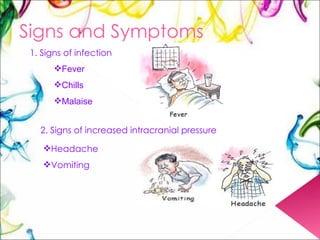
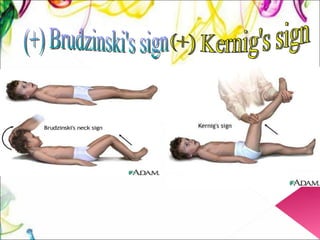
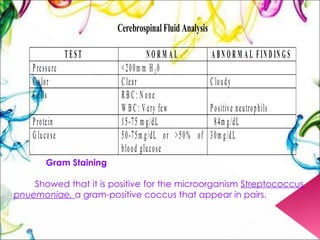
The document summarizes a case presentation of meningitis. It describes the signs and symptoms, causes, transmission, treatment and prevention of meningitis. It then details a specific case of a 9-month-old male patient admitted with fever and convulsions who was diagnosed with meningitis caused by Streptococcus pneumoniae based on diagnostic tests.