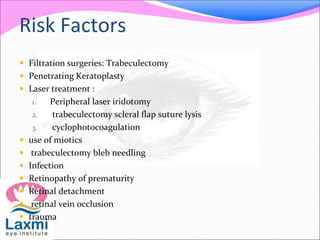
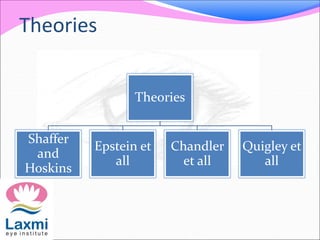
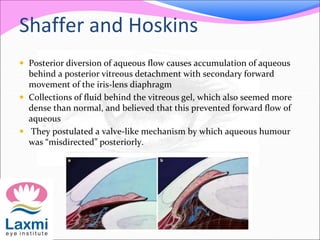
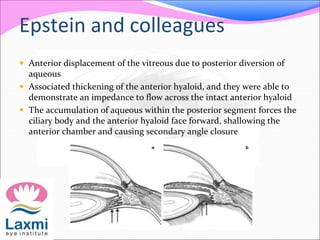
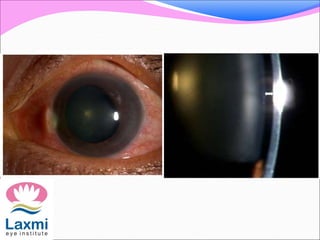
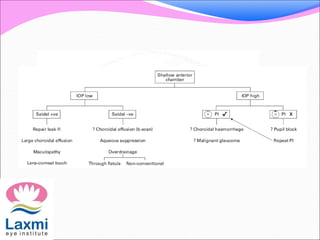
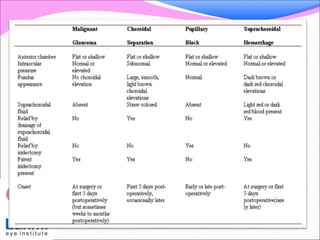
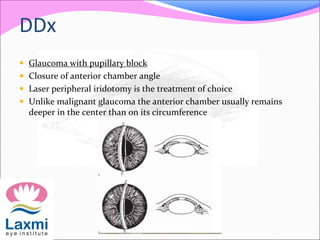
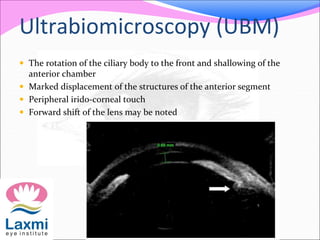
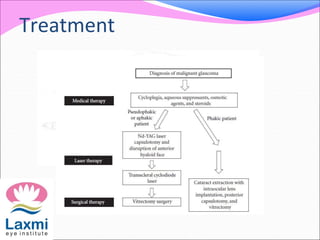
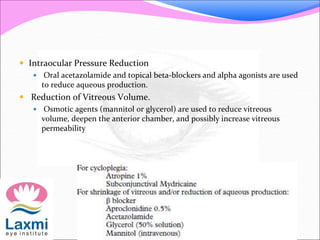
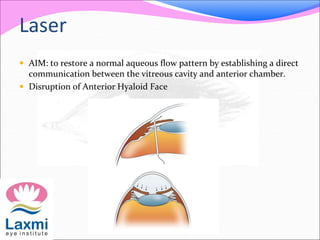
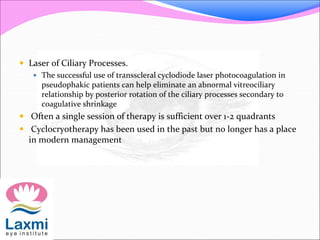
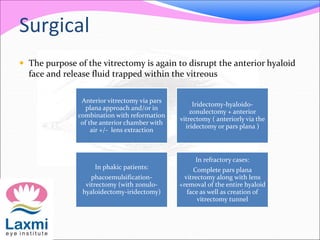
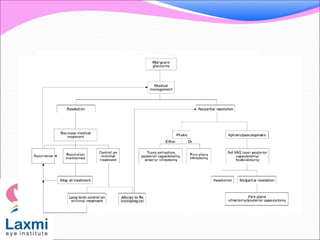
Malignant glaucoma is a complication that can occur after glaucoma filtration surgery where the anterior chamber becomes shallow despite a patent iridotomy. It is caused by abnormal accumulation of aqueous humor behind the lens and iris, causing the iris-lens diaphragm to move forward. Theories of its cause include posterior diversion of aqueous flow, anterior displacement of the vitreous, or pressure from an expanded choroid pushing the lens forward. Treatment involves cycloplegics to pull the lens back, reducing aqueous production and IOP, and sometimes laser treatment or vitrectomy surgery to disrupt the abnormal fluid buildup.