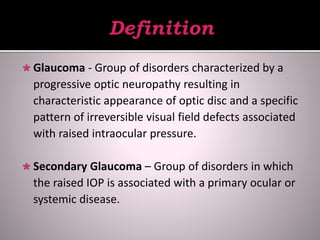
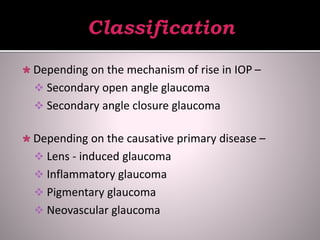
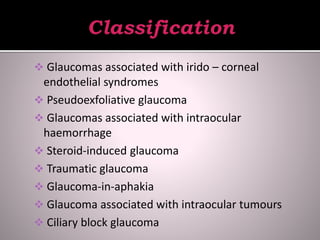
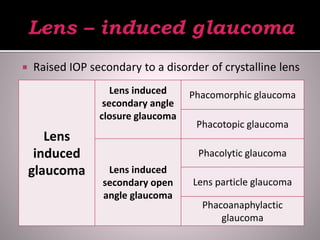
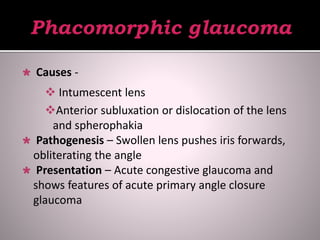
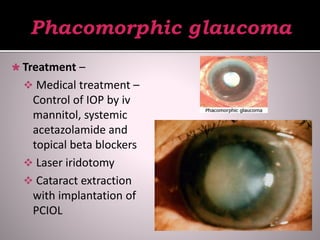
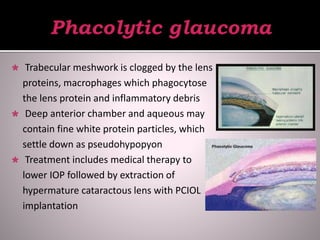
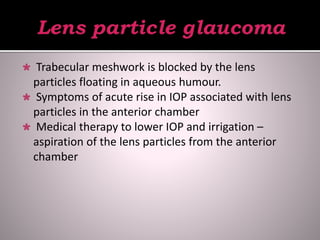
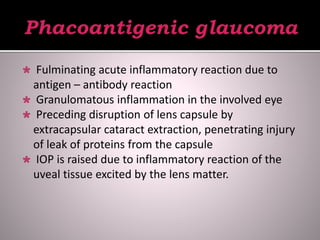
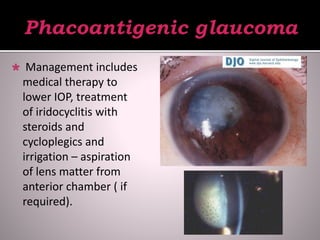
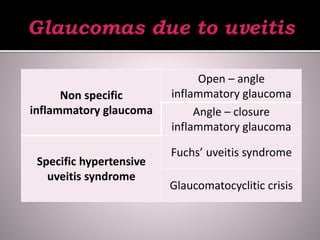
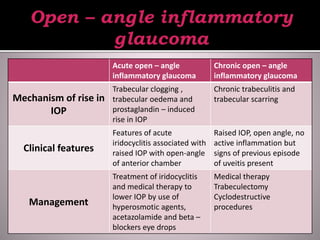
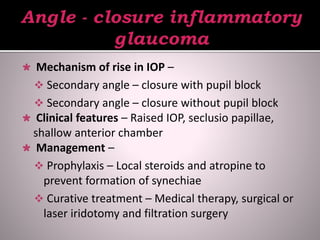
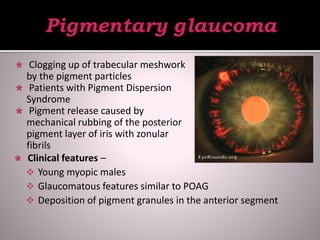
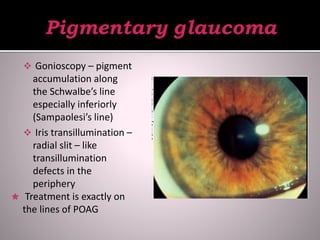
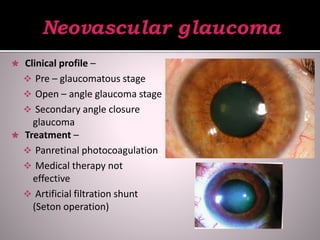
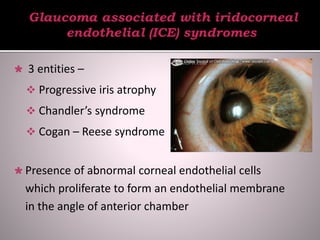
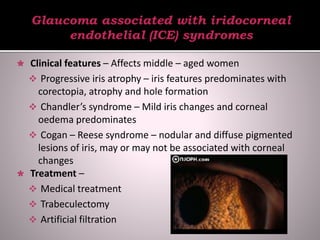
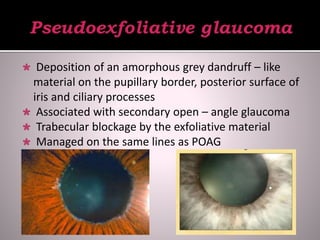
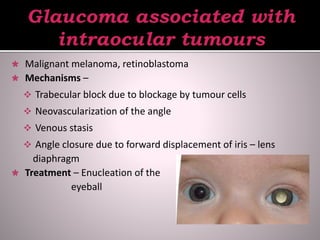
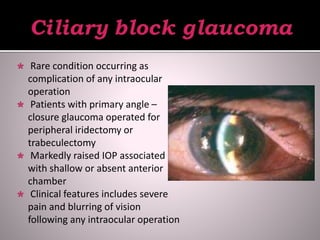
This document discusses various types of secondary glaucoma caused by underlying ocular diseases and conditions. It describes the mechanisms of increased intraocular pressure, clinical features, and treatment approaches for different forms of secondary glaucoma including lens-induced glaucoma, inflammatory glaucoma, pigmentary glaucoma, neovascular glaucoma, and steroid-induced glaucoma among others. Management involves treating the underlying condition causing secondary glaucoma as well as lowering intraocular pressure through medical, laser, or surgical means.