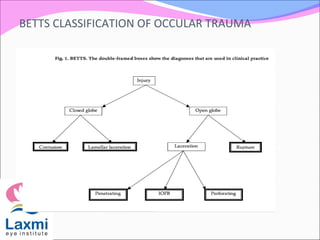
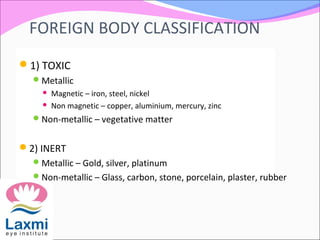
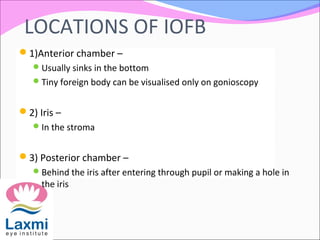
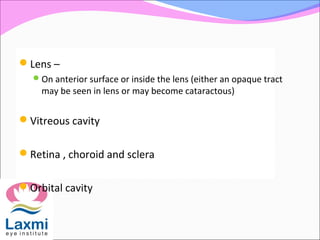
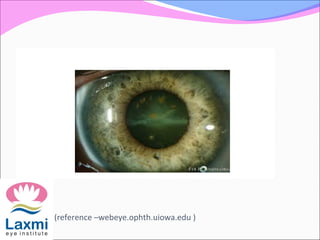
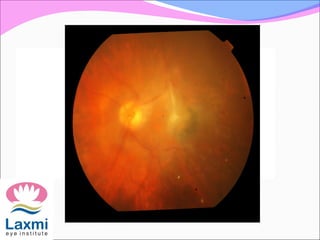
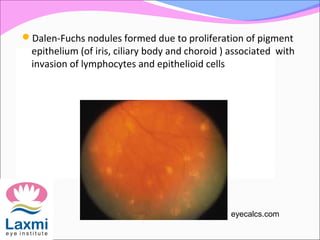
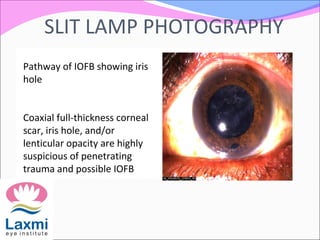
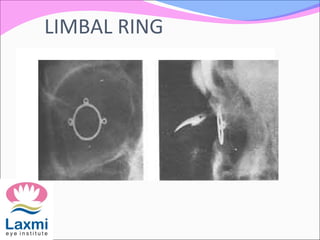
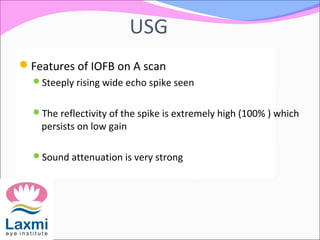
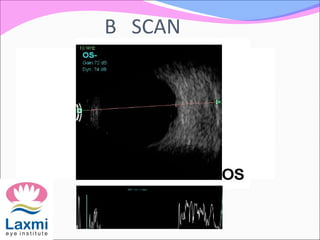
This document discusses intraocular foreign bodies (IOFBs) resulting from penetrating ocular trauma. It describes the classification of IOFBs as toxic (e.g. metallic) or inert (e.g. glass) and the various types of damage they can cause, including mechanical effects, introduction of infection, and reactions to the foreign material. Specific reactions to iron (siderosis) and copper (chalcosis) are also outlined. The locations where IOFBs can lodge in the eye are provided, as well as methods for localizing and managing retained IOFBs. Prompt removal of IOFBs is emphasized to prevent complications like endophthalmitis, secondary glaucoma, and sympathetic o