Intraoperative floppy iris syndrome (IFIS) is a complication observed during cataract surgery, often linked to the use of tamsulosin, an alpha-1 antagonist. The syndrome is characterized by iris billowing and prolapse, which increases the likelihood of surgical complications, including capsular rupture and vitreous loss. Effective management strategies such as preoperative pupil dilation with atropine and the use of intracameral alpha agonists may reduce the severity of IFIS during surgery.







![8
11. Chang DF, Campbell JR, Colin J, Schweitzer C. Prospective masked comparison of intraoperative floppy iris syndrome
severity with tamsulosin versus alfuzosin. Ophthalmology 2014;121:829-834
12. Goseki T, Shimizu K, Ishikawa H, Nishimoto H, Uga S, Nemoto N, Patil PN. Possible mechanism of intraoperative
floppy iris syndrome: a clinicopathological study. Br J Ophthalmol. 2008; 92: 1156-1158
13. Santaella RM, Destafeno JJ, Stinnett SS, et al. The effect of alpha1-adrenergic receptor antagonist tamsulosin
(Flomax) on iris dilator smooth muscle anatomy. Ophthalmology. 2010;117:1743-1749.
14. Goseki T, Ishikawa H, Ogasawara S, et al. Effects of tamsulosin and silodisin on isolated albina and pigmented
rabbit iris dilators – Possible mechanism of IFIS. J Cataract Refract Surg 2012;38: 1643-1649.
15. Masket S, Belani S. Combined preoperative topical atropine sulfate 1% and intracameral nonpreserved
epinephrine hydrochloride 1:4000 [corrected] for management of intraoperative floppy-iris syndrome. J Cataract
Refract Surg. 2007; 33:580-582.
16. Shugar, JK. Intracameral Epinephrine for Prophylaxis of IFIS [letter]. J Cataract Refract Surg 2006; 32: 1074-
1075.
17. Gurbaxani A, Packard R. Intracameral phenylephrine to prevent floppy iris syndrome during cataract surgery in
patients on tamsulosin. Eye. 2007; 21:331-332.
18. Manvikar S, Allen D. Cataract surgery management in patients taking tamsulosin. J Cataract Refract Surg 2006; 32:
1611-1614
19. Lorente R, de Rojas V, Vázquez de Parga P, et al. Intracameral Phenylephrine 1.5% for Prophylaxis against
Intraoperative Floppy Iris Syndrome: Prospective, Randomized Fellow Eye Study. Ophthalmology. 2012 Jun 16.
[Epub ahead of print]
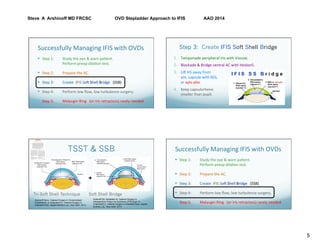
20. Arshinoff SA. Modified SST-USST for tamsulosin-associated intraocular floppy iris syndrome. J Cataract Refract
Surg 2006; 32: 559-561.
21.Chang DF. Use of Malyugin pupil expansion device for intraoperative floppy iris syndrome: Results in 30
consecutive cases. J Cataract Refract Surg 2008;34:835-841.](https://image.slidesharecdn.com/talksofinterest-floppyiris-170418085555/85/Floppy-iris-Syndrome-9-320.jpg)