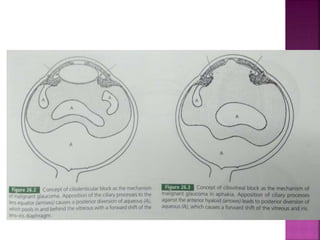
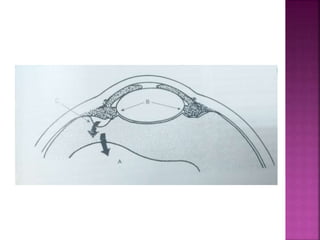
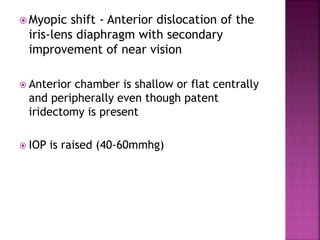
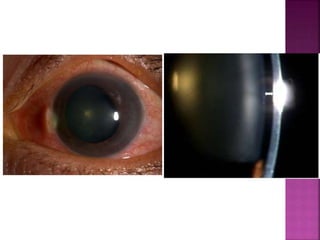
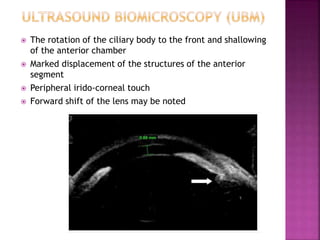
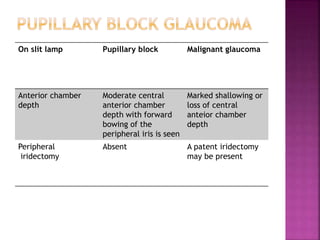
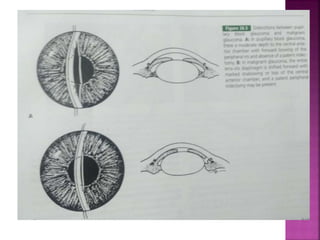
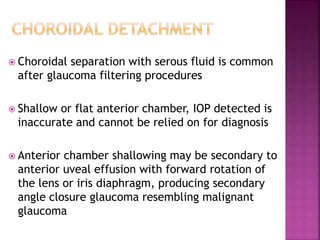
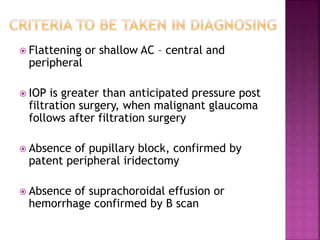
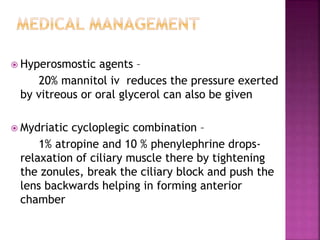
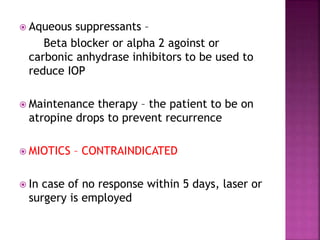
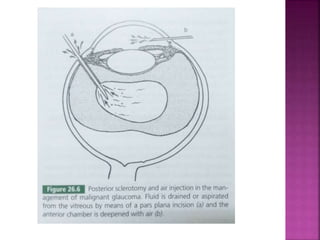
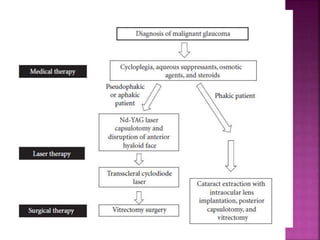
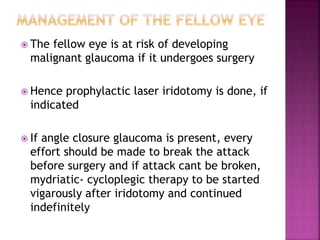
This document discusses malignant glaucoma, beginning with definitions and history. It describes the mechanisms behind malignant glaucoma as abnormal forward shifting of the iris-lens diaphragm. Clinical features include increased eye pressure despite patent iridotomy and shallowing of the anterior chamber. Differential diagnosis and management options are provided, including medical therapy, laser treatment, and surgeries like posterior sclerotomy with air injection. The fellow eye is also at risk and may require prophylactic treatment.