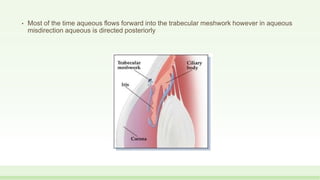
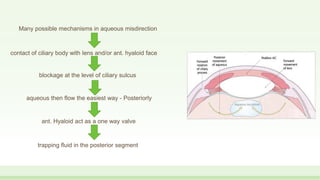
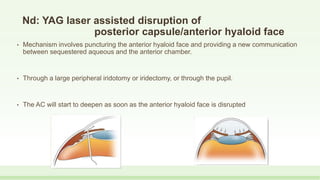
This document discusses malignant glaucoma, a condition characterized by a shallow anterior chamber and elevated intraocular pressure despite a patent iridectomy. It occurs most commonly after glaucoma surgery. Several theories exist for its pathogenesis, involving aqueous misdirection posteriorly due to cilio-lenticular or cilio-vitreal blocks. Clinical features, diagnosis, differential diagnosis, and management approaches are described, including medical therapy with cycloplegics and hyperosmotics, laser treatments, and surgical interventions like vitrectomy. Preventing recurrence in the fellow eye is also addressed.