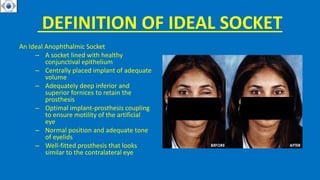
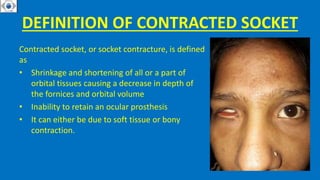
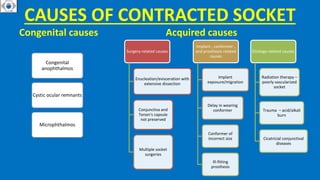
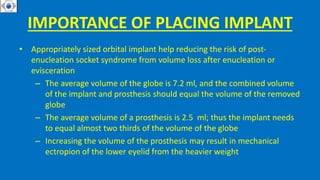
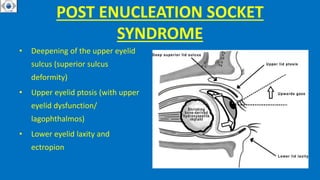
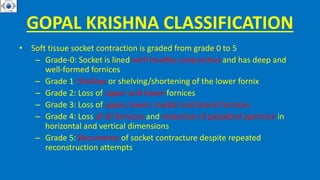
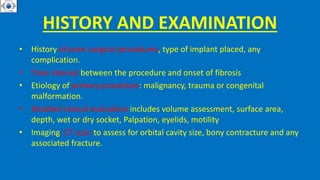
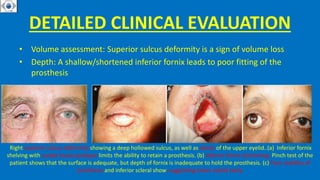
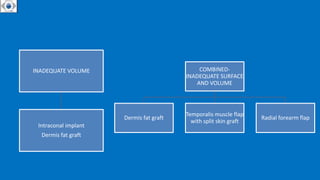
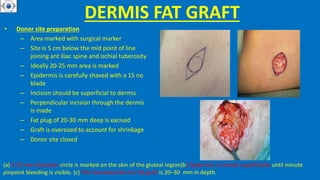
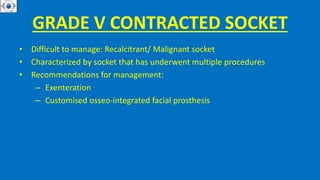
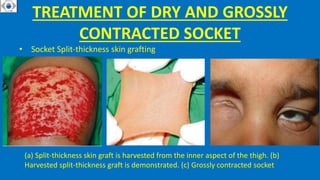
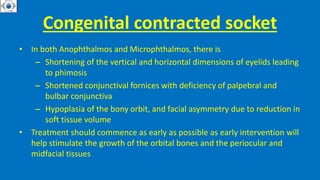
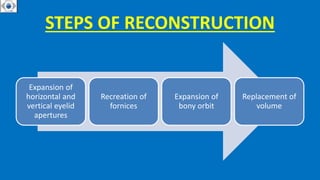
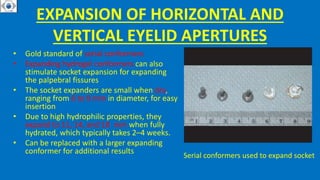
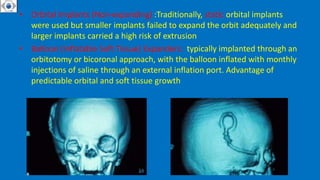
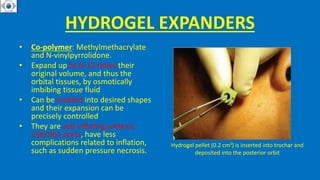
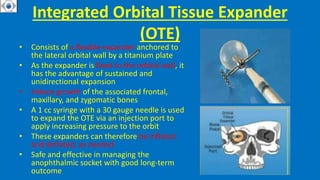
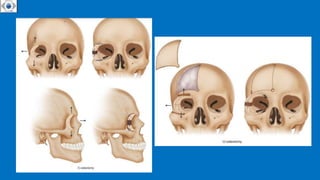
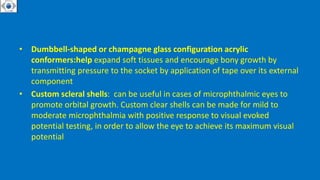
This document discusses the definition, causes, classification, and management of contracted sockets after eye removal. A contracted socket is when the orbital tissues shrink, decreasing the depth of the eye socket and preventing an artificial eye from fitting properly. Common causes include previous extensive eye surgery, delays in socket treatment, radiation therapy, and trauma. Contracted sockets are classified based on the degree of fornix involvement and palpebral aperture changes. Management aims to restore socket depth and volume through techniques like fornix reconstruction with grafts, eyelid tightening procedures, dermis fat grafts, and muscle flaps.