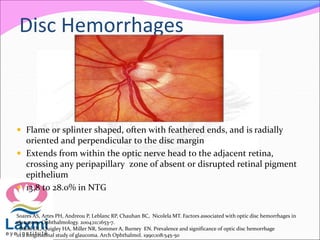
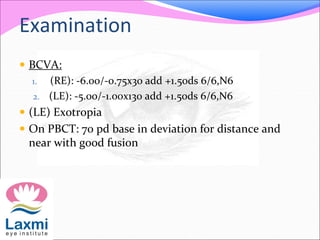
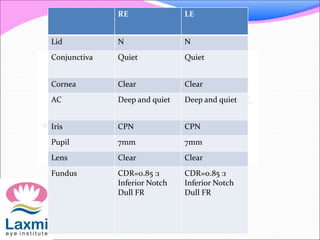
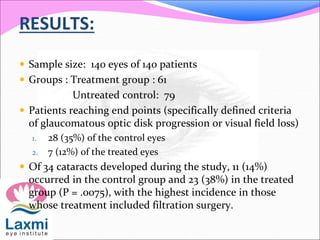
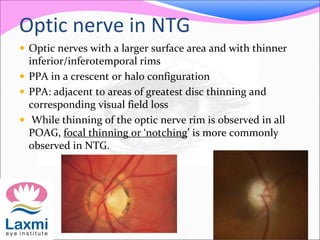
This document summarizes a presentation on normal tension glaucoma (NTG). It begins with an introduction defining NTG as open-angle glaucoma with characteristic optic nerve damage and visual field defects in patients with consistently low intraocular pressure (IOP) below 21 mmHg. It then describes a case presentation of a 47-year-old female patient. The remainder of the document discusses the history, examination, investigations, differential diagnosis, management, pathogenesis involving both IOP-dependent and independent factors, and epidemiology of NTG. Key points are that lowering IOP through medication or surgery can help prevent progression even in NTG, and that NTG may have an underlying vascular component involving low ocular perfusion pressure
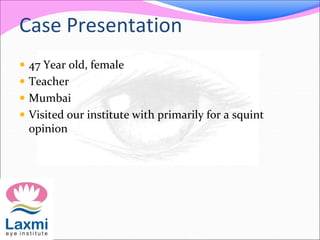
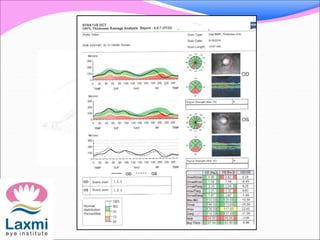
![Mean Ocular Perfusion Pressure
Ocular perfusion pressure (OPP), the relationship
between systemic blood pressure and IOP
Mean ocular perfusion pressure(MOPP)
MOPP = 2/3 [DBP + 1/3(SBP – DBP)] – IOP
Risk factor for open-angle glaucoma.
Because low blood pressure lets OPP drop, and low OPP is
similar to elevated IOP,hence it has consistently and
strongly been associated with OAG.](https://image.slidesharecdn.com/normaltensionglaucoma-140715225132-phpapp01/85/Normal-tension-glaucoma-23-320.jpg)

![Acquired pits of optic nerve
Acquired pits of optic nerve [APON] which are
thought to be due to focal loss of neuroretinal rim
tissue and shown as localised excavations of the
lamina cribrosa, are more frequent in NTG.
More prevalent in lower pressure glaucoma than in
higher pressure glaucoma.
Inferior part of disc> Superior
Acquired pits of the optic nerve in glaucoma: prevalence and associated visual field loss.
Nduaguba C1, Ugurlu S, Caprioli J.](https://image.slidesharecdn.com/normaltensionglaucoma-140715225132-phpapp01/85/Normal-tension-glaucoma-32-320.jpg)