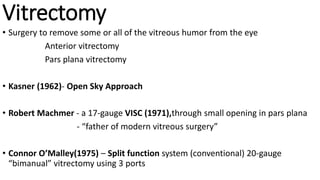
This document summarizes instrumentation, techniques, and outcomes of microincision vitrectomy surgery (MIVS). It describes the evolution from larger 20-gauge vitrectomy systems to smaller 23-gauge and 25-gauge systems. The key benefits of smaller gauges include reduced post-operative inflammation, astigmatism, and risk of retinal breaks. While 25-gauge surgery enables a self-sealing sutureless approach, it has limitations such as slower flow rates and more difficult intraocular maneuvers compared to 23-gauge which provides an optimal balance between benefits and technical ease.