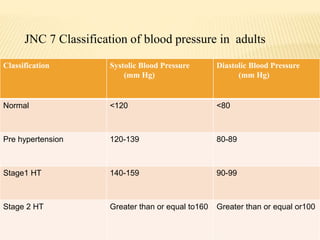
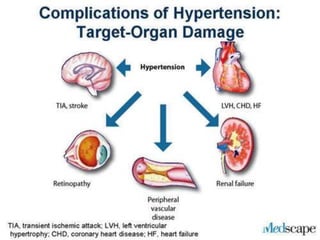
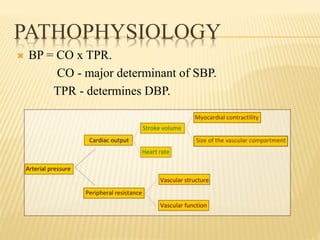
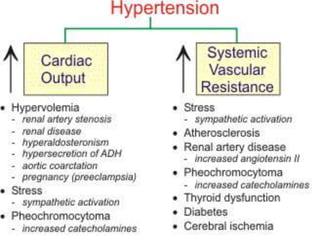
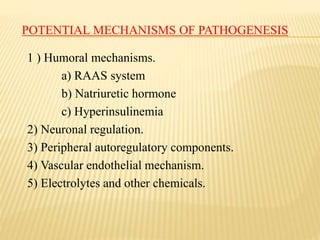
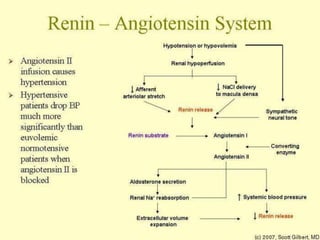
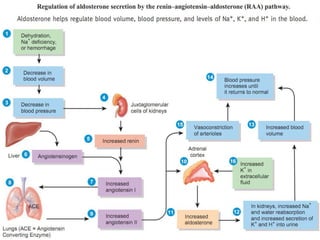
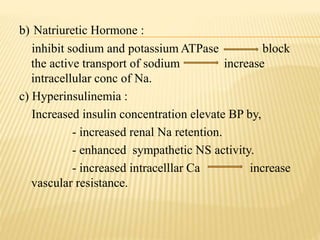
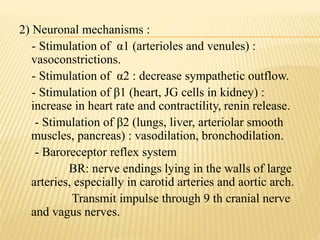
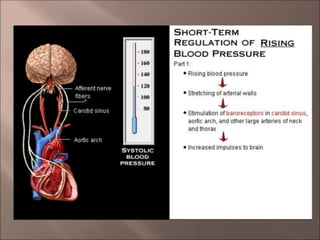
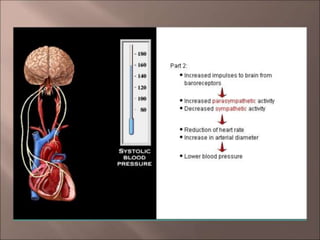
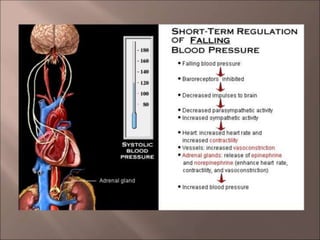
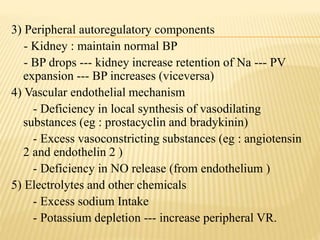
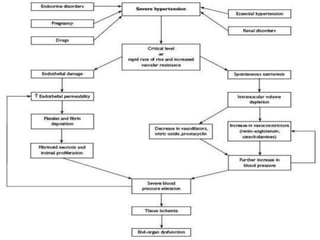
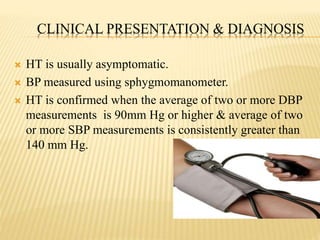
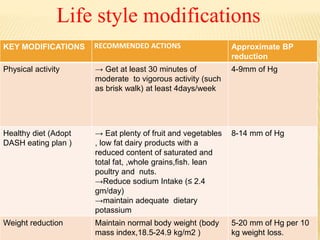
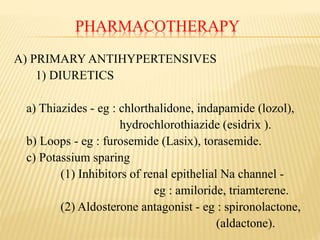
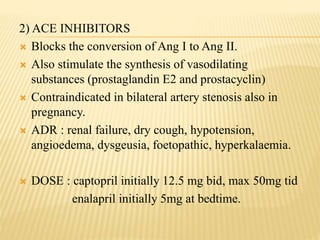
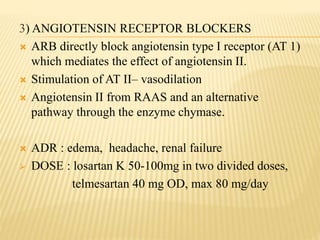
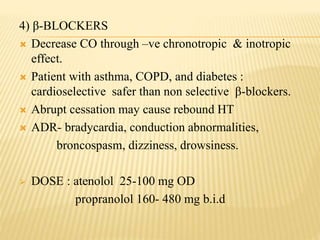
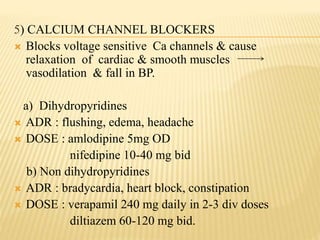
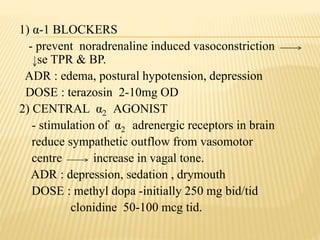
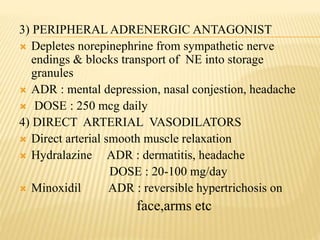
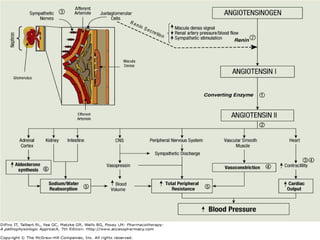
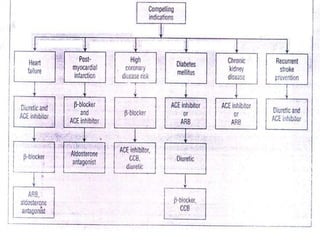
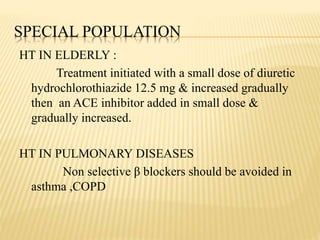
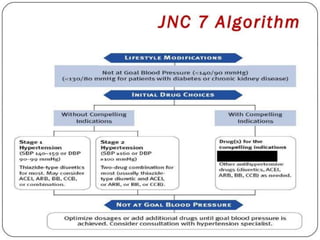
The document discusses hypertension, including its definition, classification, epidemiology, types, etiology, pathophysiology, clinical presentation, diagnosis, and management. Hypertension is defined as elevated blood pressure above 140/90 mmHg and can be essential or secondary. Common types include essential, secondary, white coat, and isolated systolic hypertension. Lifestyle modifications and medications are used to treat hypertension, with drug classes including diuretics, ACE inhibitors, ARBs, beta-blockers, calcium channel blockers, and others. The goal of treatment is to control blood pressure and reduce long term health risks.