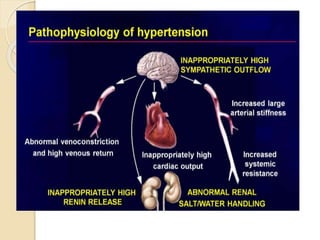
The document discusses hypertension, defining it as a condition characterized by sustained high blood pressure, and explores its various types, risk factors, and pathophysiology. It details clinical manifestations, assessment methods, and management strategies, including lifestyle changes and pharmacological treatments. Additionally, it emphasizes the importance of monitoring and early intervention to prevent complications associated with hypertension.



![ASSESSMENT AND
DIAGNOSTIC EVALUATION
History collection and physical examination: The retinas and
other related part are examined, and laboratory studies are
performed to assess possible target organ damage.
Para clinical examinations: Routine examinations include:
urinalysis, blood chemistry (ie, analysis of sodium, potassium,
creatinine,
fasting glucose
Total and high-density lipoprotein [HDL] cholesterol levels),
lead electrocardiogram.
Left ventricular hypertrophy can be assessed by echocardiography.
Renal damage may be suggested by elevations in BUN and
creatinine levels or by microalbuminuria or macroalbuminuria.
Additional studies, such as creatinine clearance, renin level, urine
tests, and 24-hour urine protein, may be performed](https://image.slidesharecdn.com/hypertension-220826193537-cc726fcd/85/hypertension-pptx-15-320.jpg)

![HYPERTENSIVE CRISES
Hypertensive Urgency
It is a situation in which there is acute
severe elevation in blood pressure above
180/120mmHg without evidence of end
stage organ damage.
Hypertensive urgencies are managed with
oral doses of fast-acting agents such as
loop diuretics (bumetanide [Bumex],
furosemide [Lasix]), beta-blockers
propranolol (Inderal), Metoprolol
(Lopressor), Nadolol (Corgard),](https://image.slidesharecdn.com/hypertension-220826193537-cc726fcd/85/hypertension-pptx-37-320.jpg)