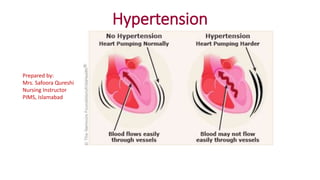
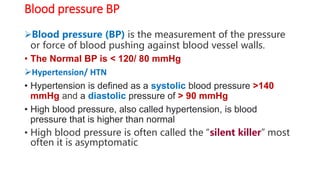
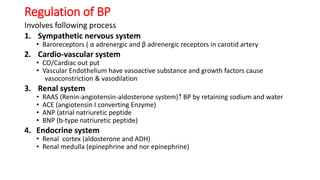
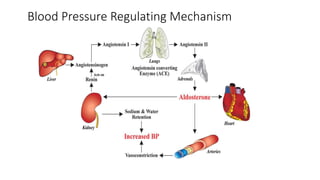
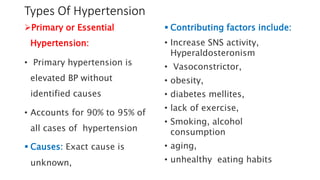
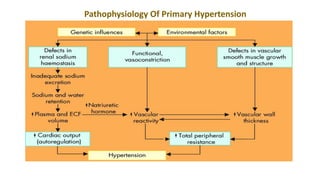
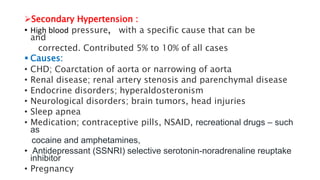
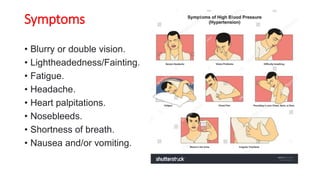
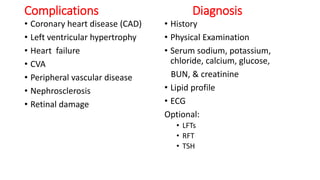
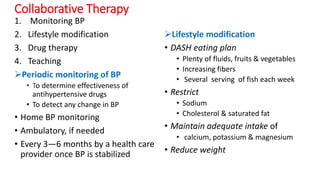
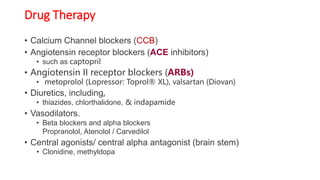
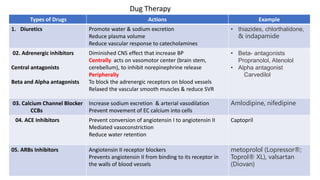
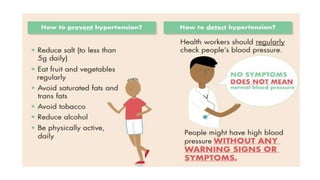
This document discusses hypertension (high blood pressure) and its causes, symptoms, diagnosis, and treatment. It defines hypertension as a blood pressure higher than 140/90 mmHg and identifies factors that can lead to primary (essential) hypertension in 90-95% of cases, like increased sympathetic nervous system activity. Symptoms of hypertension are often vague. Treatment involves lifestyle modifications like diet, exercise, smoking cessation, and stress management as well as prescription drugs like diuretics, beta blockers, ACE inhibitors, and calcium channel blockers to control blood pressure. Patient education focuses on understanding the condition, preventative measures, lifestyle changes, medication management, and the importance of follow up.