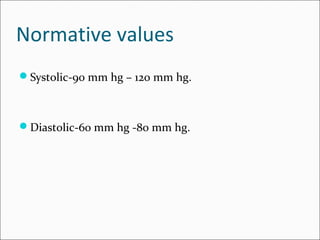
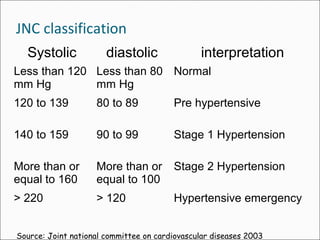
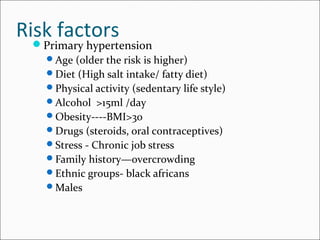
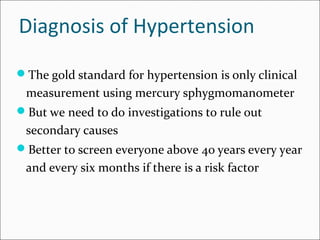
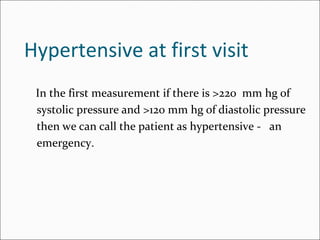
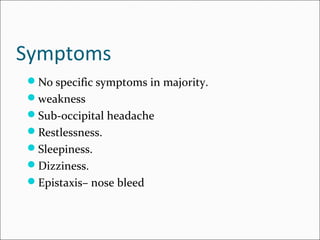
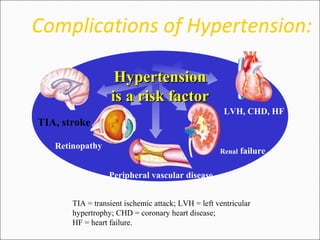
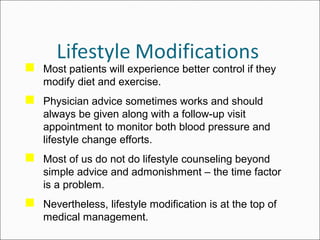
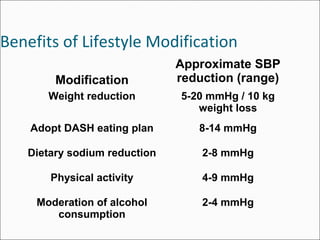
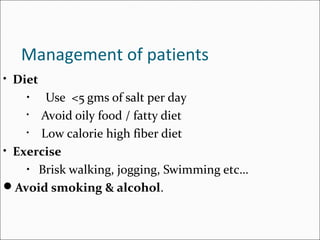
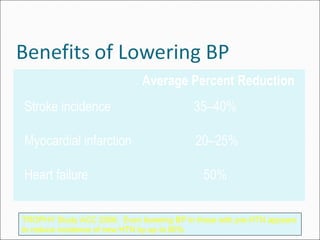
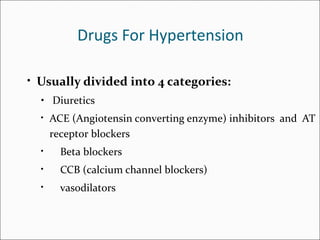
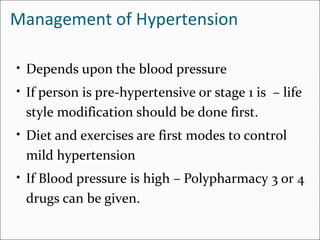
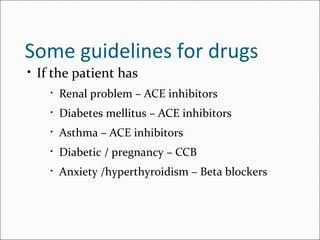
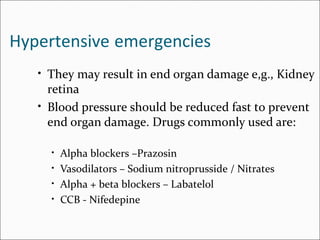
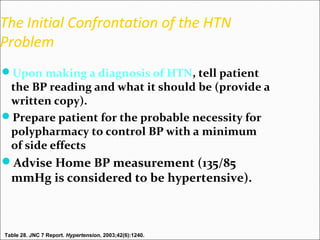
Hypertension, also known as high blood pressure, is defined as a systolic blood pressure above 140 mmHg or a diastolic blood pressure above 90 mmHg. It is a major health problem affecting over 30% of adults in the US. While most cases of hypertension have no known cause, risk factors include age, diet, physical activity levels, obesity, and family history. Left untreated, hypertension can lead to serious health complications like heart attack, stroke, kidney failure, and retinal damage. Lifestyle modifications including reduced salt intake, increased physical activity, and weight loss are recommended as first-line treatment, along with medication if needed to control blood pressure.