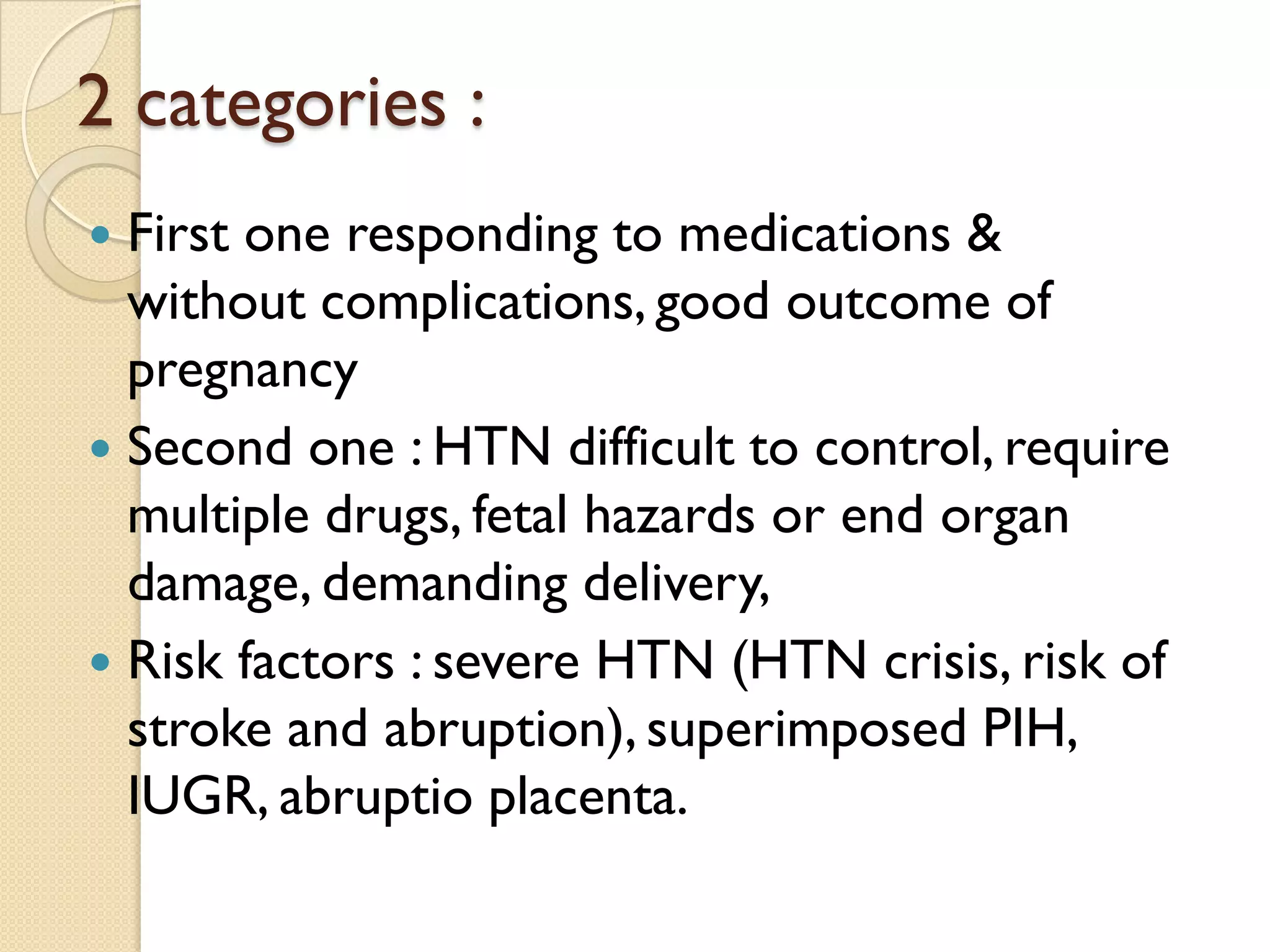
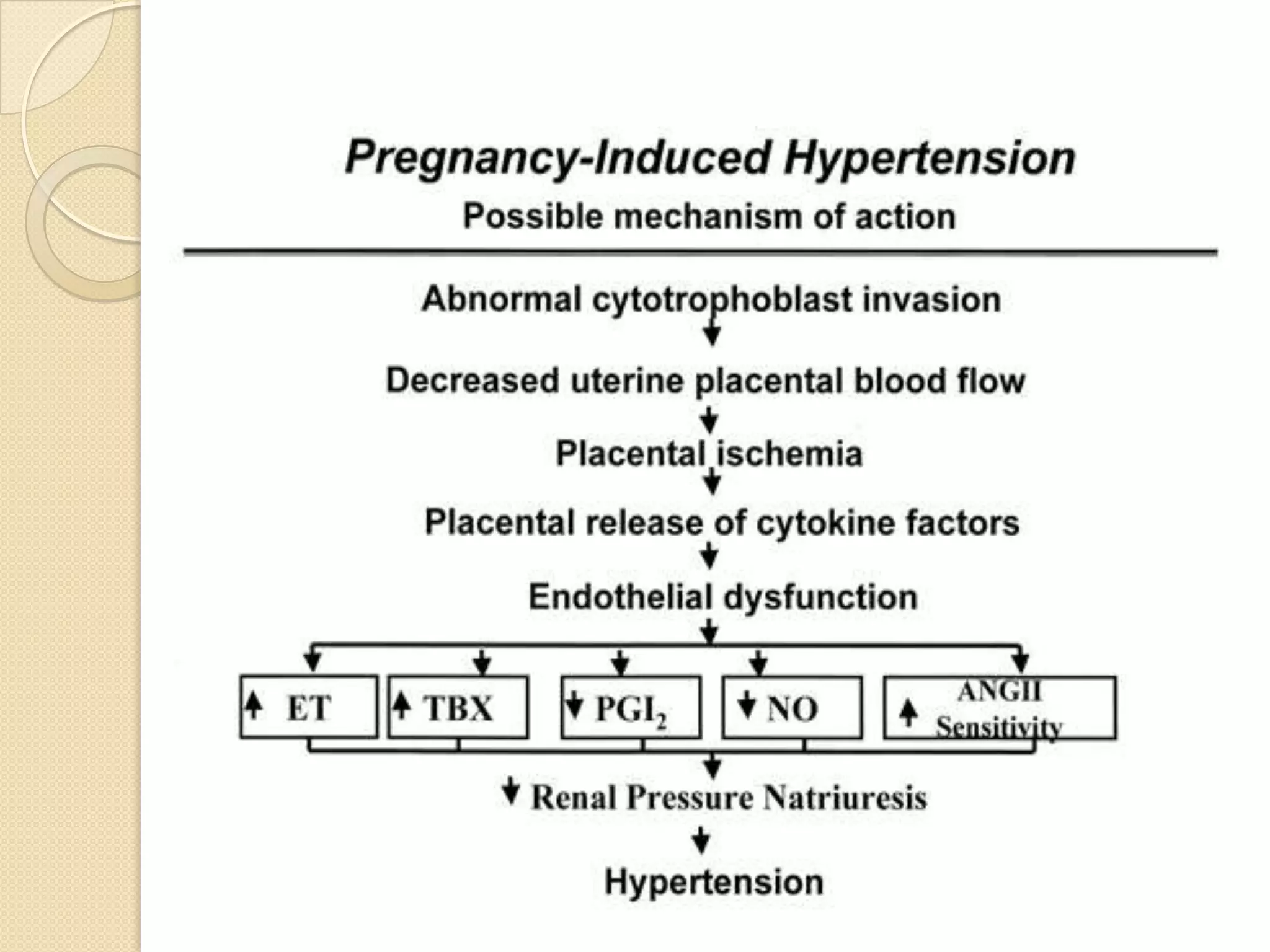
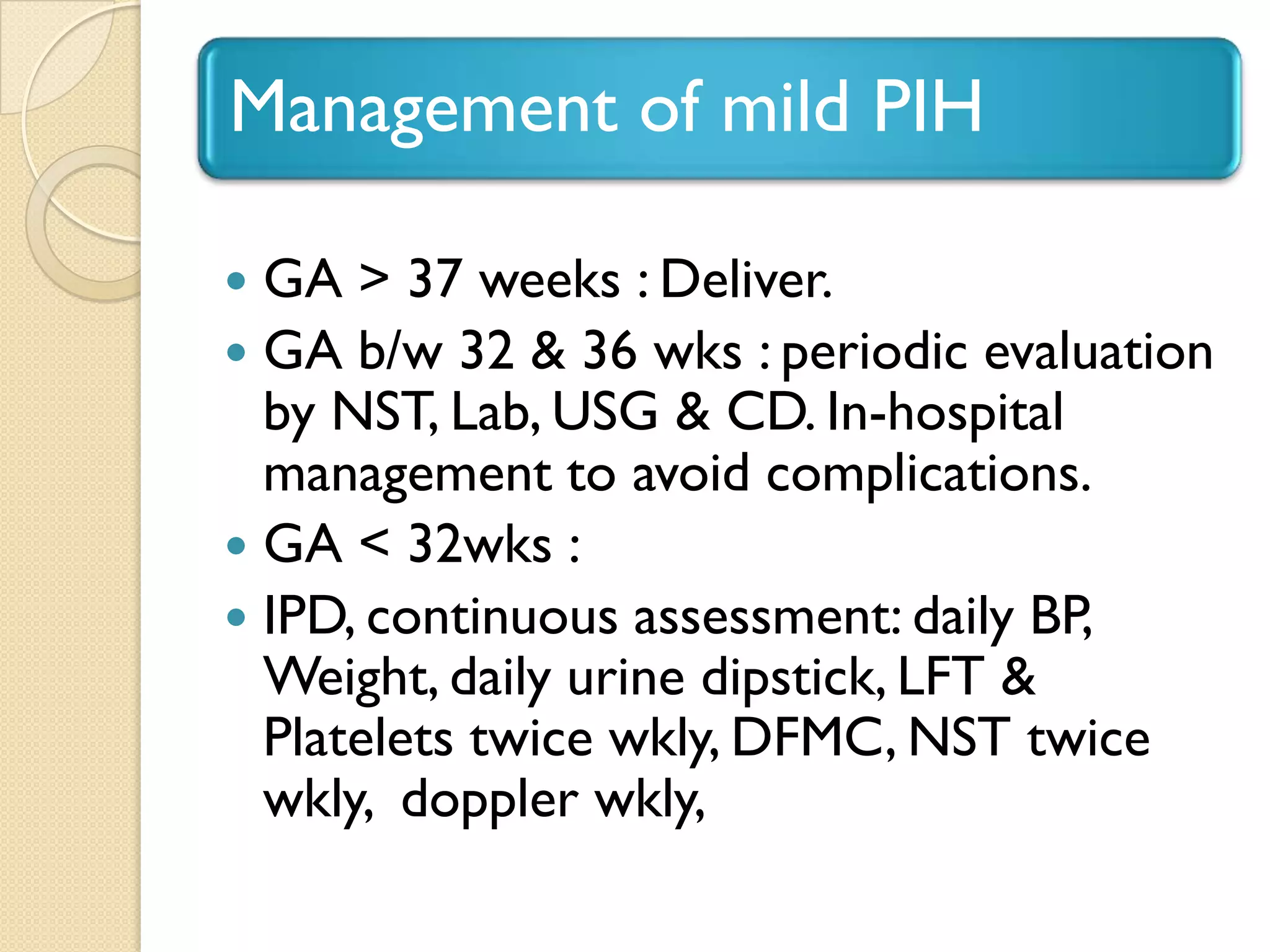
This document discusses pregnancy induced hypertension (PIH), also known as preeclampsia. PIH is a multisystem disorder characterized by high blood pressure and protein in the urine that develops during pregnancy. It can lead to serious complications for both the mother and baby if untreated. The document covers the definition, classification, signs and symptoms, risk factors, pathogenesis, diagnosis, and management of mild and severe cases of PIH.