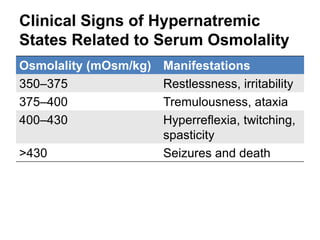
This document discusses hypernatremia, defined as a serum sodium level greater than 150 mEq/L. It describes the normal extracellular and intracellular fluid compartments and how they are affected by hypernatremia. Clinical signs of hypernatremia range from restlessness to seizures and death depending on the serum osmolality level. Common causes include inadequate water intake, excessive sodium intake, renal or GI losses. Treatment involves volume repletion first with isotonic fluids followed by a gradual decrease in sodium levels with hypotonic fluids over 1-2 days. Free water deficits are calculated to determine fluid replacement volumes needed.
![Hypernatremia
[Na]> 150 mEq/L](https://image.slidesharecdn.com/hypernatremia-130331071614-phpapp01/85/Hypernatremia-1-320.jpg)




![Diabetes Insipidus
Diabetes insipidus is characterized by the
failure of central or peripheral ADH
response.
Urine osmolality is low (200 to 300
mOsm/kg, with urinary [Na+] of 60 to 100
mEq/kg)](https://image.slidesharecdn.com/hypernatremia-130331071614-phpapp01/85/Hypernatremia-7-320.jpg)
![Treatment
The cornerstone of treatment is volume repletion.
Volume should be replaced first with NS or lactated
Ringer's solution.
Some practitioners inappropriately fear using NS solution
from concern that an [Na+] of 154 mEq/L exceeds normal
serum [Na+]. However, in most hypernatremic states,
there is a total body [Na+] deficit, and the use of NS
allows a more gradual decrease in serum [Na+].
Once perfusion has been established, the solution should
be converted to 0.45% saline or another hypotonic
solution until the urine output is at least 0.5 mL/kg/h.
The reduction in [Na+] should not exceed 10~15
mEq/L per day.](https://image.slidesharecdn.com/hypernatremia-130331071614-phpapp01/85/Hypernatremia-8-320.jpg)

![Calculation of Free Water Deficit
measured[Na ]
TBW 0.6 1
desired[Na ]
Replacement Volume = TBW deficit × 1/(1-X)
X= [Na+] of resuscitation fluid / [Na+] of isotonic saline](https://image.slidesharecdn.com/hypernatremia-130331071614-phpapp01/85/Hypernatremia-10-320.jpg)
![70 公斤的成人,抽血發現 [Na+] 160 mEq/L
計算式:
TBW deficit = 0.6 ×70× [160/140-1]= 6 L
若使用 0.45NaCl 做為輸液
Replacement volume = 6 × 1/ (1-½)=12 L
水分缺損要在 48小時 補足
點滴速度大約每小時要 250 mL](https://image.slidesharecdn.com/hypernatremia-130331071614-phpapp01/85/Hypernatremia-11-320.jpg)
