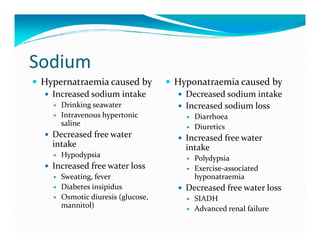
The human body is approximately 60% water, with total body water being around 42L. The water is divided into intracellular fluid (28L), interstitial fluid (10L), plasma (3L), and transcellular fluid (1L). The major ions in extracellular fluid are Na+ (142 mmol/L), Cl- (105 mmol/L), and HCO3- (27 mmol/L). In intracellular fluid, the major ions are K+ (160 mmol/L) and phosphate (100 mmol/L). Plasma osmolarity is tightly regulated at around 290 mosm/L through mechanisms involving sodium, water, the renin-angiotensin-aldosterone system,




![Plasma osmolarity
Plasma osmolarity Molarity
290 mosmol/ℓ 5 5 4
11
Measured vs Estimated 25
Sodium
Chloride
2x([Na+] + [K+]) + Urea 140
Bicarbonate
Glucose
+ Glucose Urea
Tonicity 100 Potassium
Other
Active osmolyte /
Penetrating solute
Cell](https://image.slidesharecdn.com/lomwaterelectrolyte2013-130207230556-phpapp01/85/water-electrolyte-6-320.jpg)




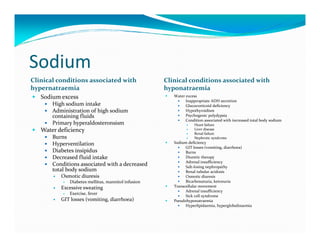
![Potassium
Predominant intracellular cation
Only 2% of potassium is extracellular [K+] = 4 [K+] = 150
Major role of K+ is to create a membrane K+
potential in excitable cells (nerve, Na+
muscle, β-cells of pancreas)
Plasma potassium negatively regulated
by aldosterone ―
+ CELL
Hypokalaemia hyperpolarises cells -90mV
Muscle weakness
Decreased cardiac excitability, cardiac
arrest
Decreased insulin secretion
Hyperkalaemia depolarises cells voltage-gated
Na channel,
Cardiac arrhythmias, ventricular opens once
fibrillation membrane
potential falls
to -60mV](https://image.slidesharecdn.com/lomwaterelectrolyte2013-130207230556-phpapp01/85/water-electrolyte-13-320.jpg)



