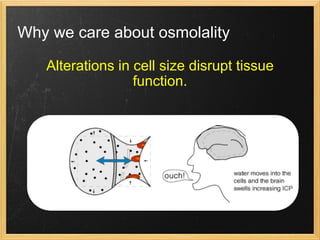
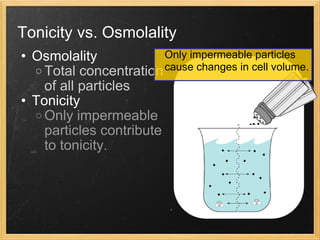
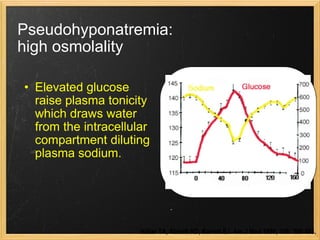
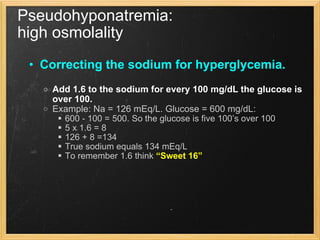
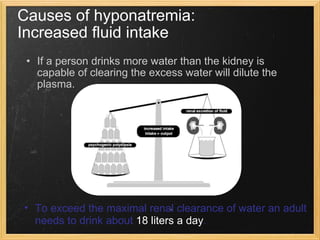
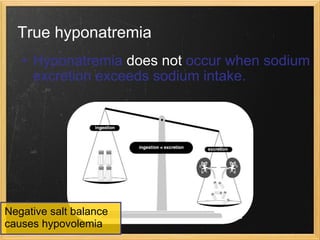
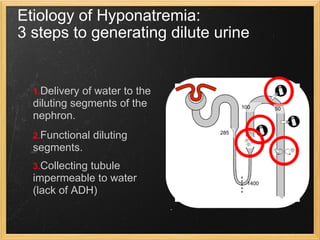
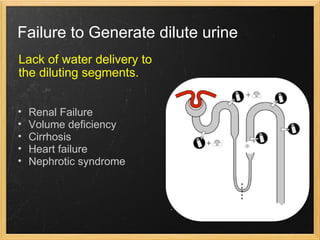
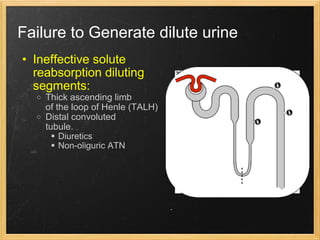
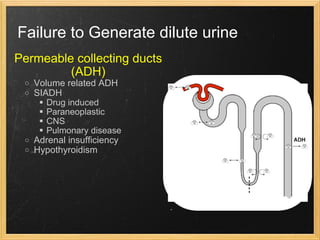
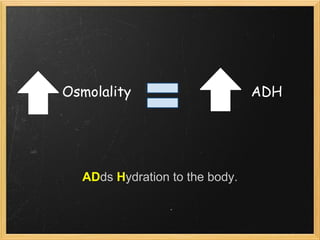
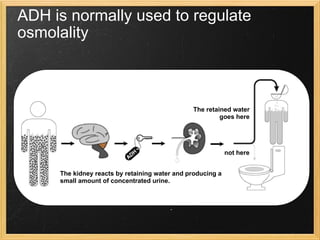
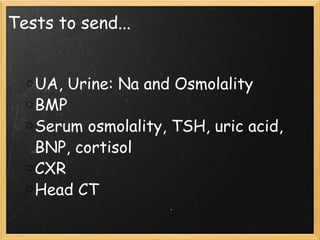
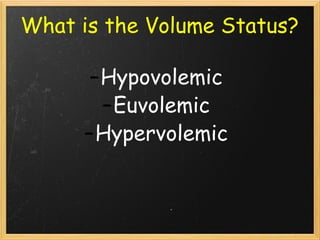
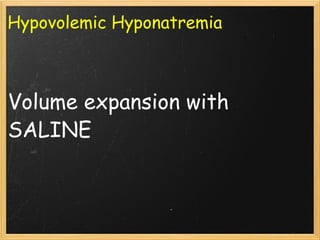
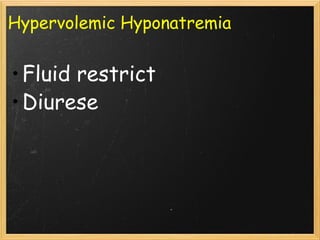
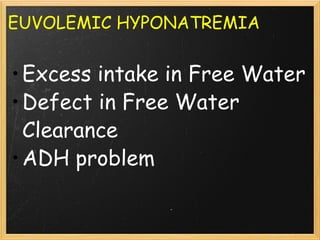
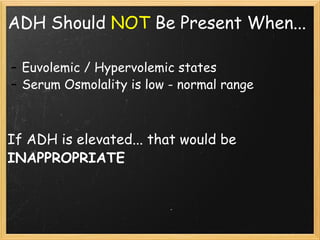
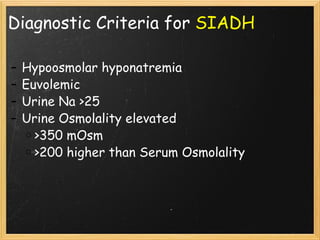
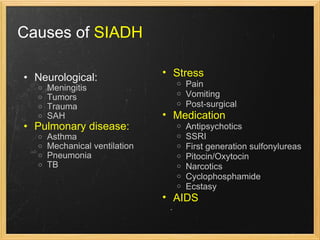
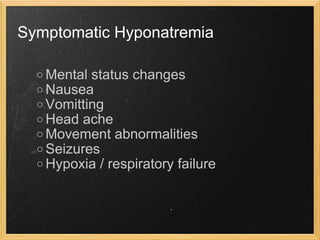
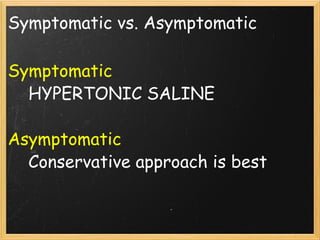
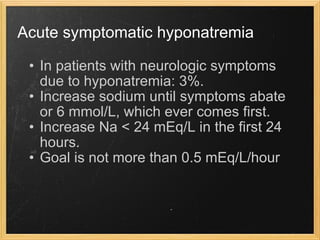
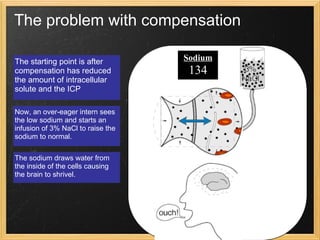
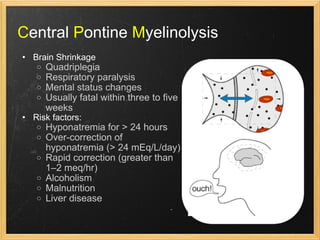
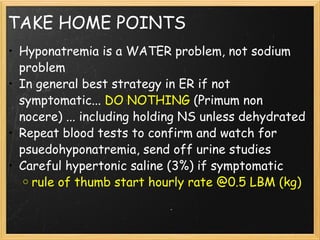
This document discusses hyponatremia, which is caused by an excess of water in the body relative to sodium. It describes how sodium levels indicate tonicity rather than just osmolality. Pseudohyponatremia can occur with hyperglycemia. Treatment depends on whether the patient is hypovolemic, euvolemic, or hypervolemic. Symptomatic hyponatremia should be treated cautiously with hypertonic saline to avoid complications like central pontine myelinolysis.