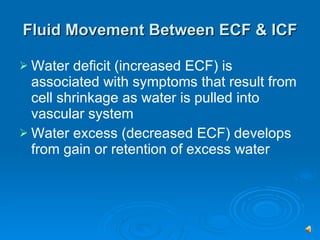
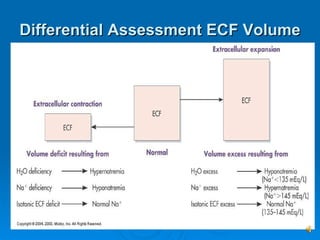
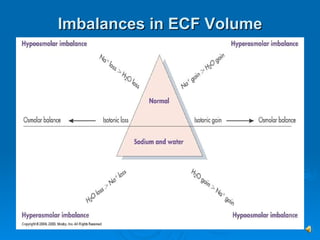
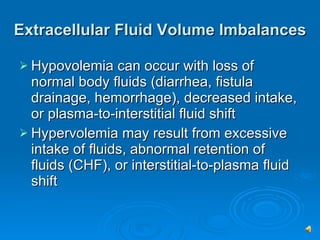
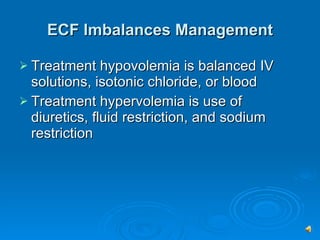
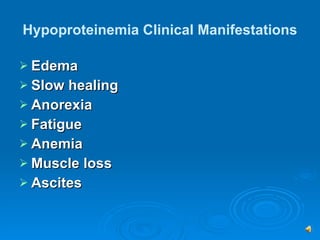
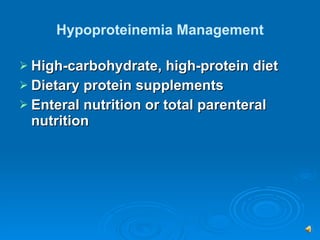
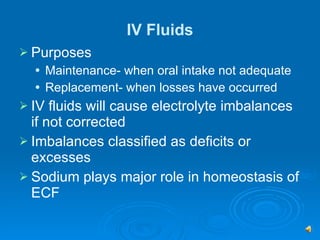
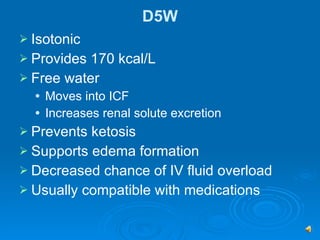
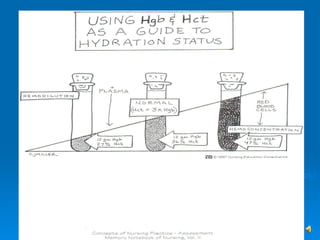
This document discusses fluid imbalances and extracellular fluid volume imbalances. It describes hypovolemia as a deficiency in fluid volume that can result from loss of fluids or decreased intake. Hypervolemia is an excess fluid volume that may occur from excessive fluid intake or abnormal fluid retention. Nursing management for hypervolemia focuses on excess fluid volume, while management for hypovolemia addresses deficient fluid volume and potential complications like hypovolemic shock. The document also covers protein imbalances like hypoproteinemia and treatments like high protein diets or IV fluids.