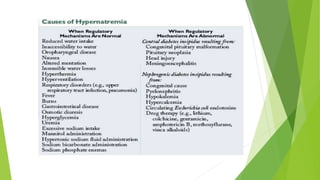
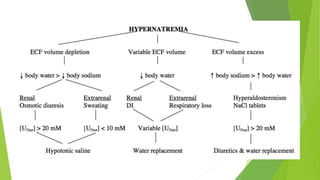
Hypernatremia is defined as a serum sodium concentration exceeding 145 mmol/L. It can be caused by hypotonic fluid deficits from renal or nonrenal losses, pure water deficits from inadequate intake or increased losses, or hypertonic sodium gains. The goals of management are to identify the underlying cause, correct any volume disturbances, and slowly correct the hypernatremia to prevent brain injury. For acute hypernatremia, the serum sodium should be decreased by 2-3 mmol/L per hour until symptoms resolve. Chronic hypernatremia should be corrected more slowly by 0.5 mmol/L per hour. The prognosis depends on factors like blood pressure, pH, and the severity and duration of hypernatrem







![Loss of hypotonic fluid (loss of water in
excess of electrolytes)
Renal hypotonic fluid loss results from anything that will interfere with the
ability of the kidney to concentrate the urine or osmotic diuresis:
Diuretic drugs (loop and thiazide diuretics)
Osmotic diuresis (hyperglycemia, mannitol, urea [high-protein tube feeding])
Postobstructive diuresis
Diuretic phase of acute tubular necrosis
Nonrenal hypotonic fluid loss can result from any of the following:
GI – Vomiting, diarrhea, lactulose, cathartics, nasogastric suction,
gastrointestinal fluid drains, and fistulas
Cutaneous – Sweating (extreme sports, marathon runs), burn injuries](https://image.slidesharecdn.com/hypernatremia-220317102916/85/Hypernatremia-8-320.jpg)