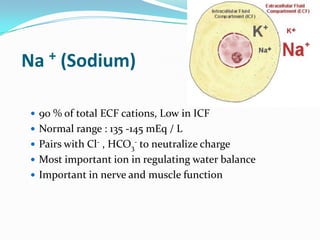
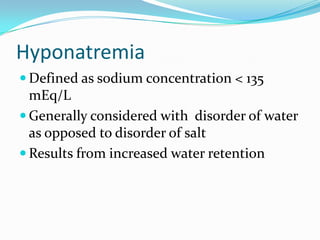
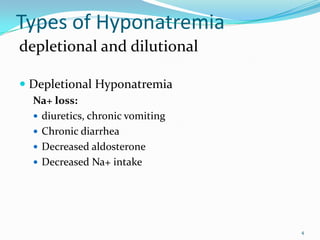
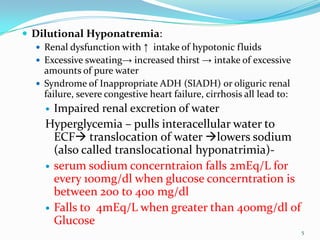
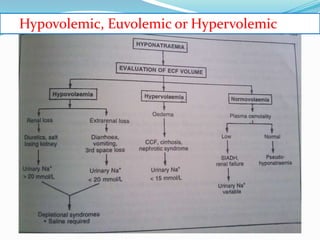
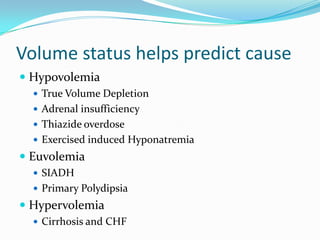
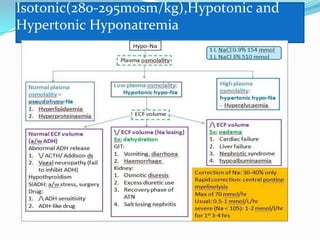
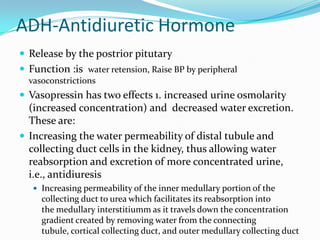
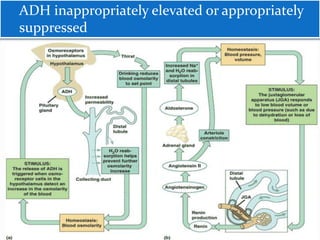
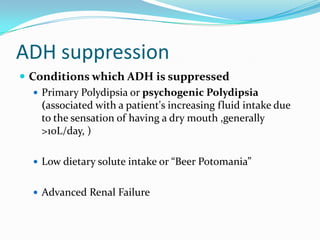
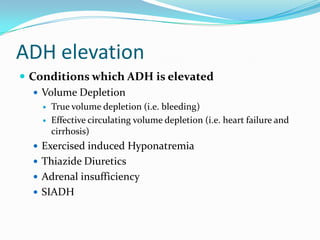
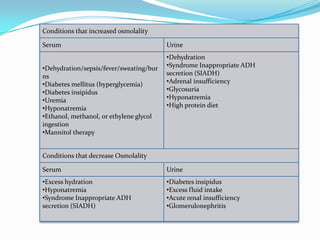
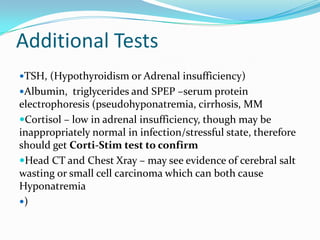
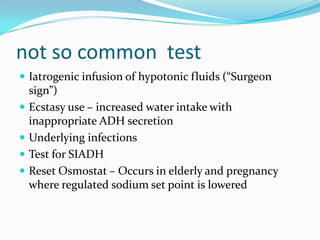
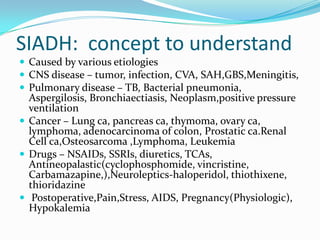
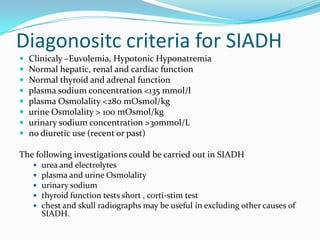
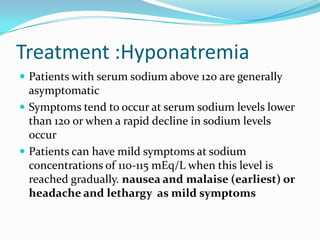
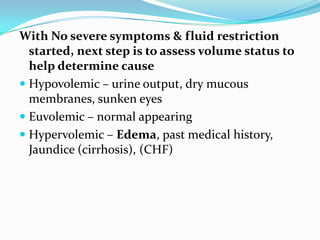
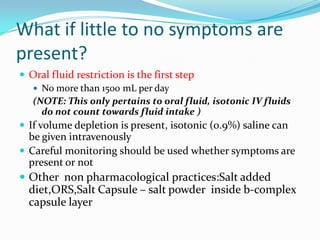
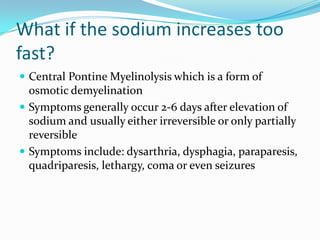
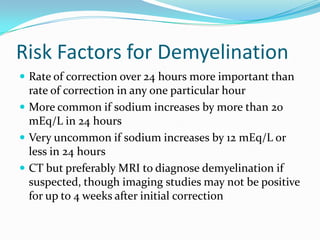
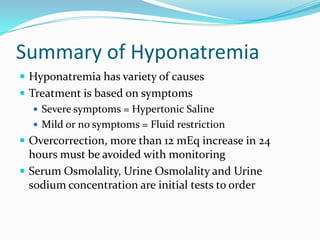
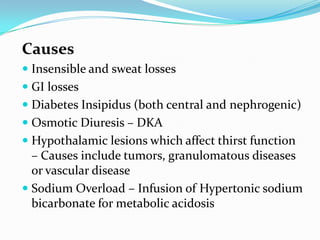
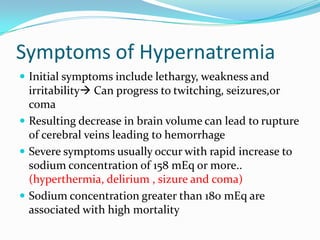
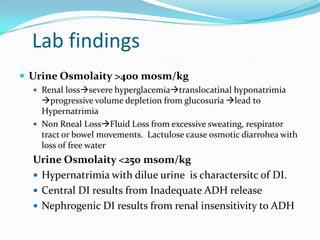
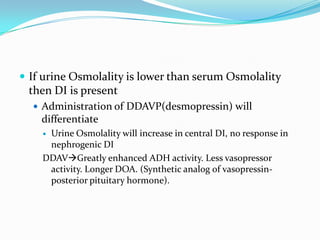
This document discusses hyponatremia and hypernatremia. It defines hyponatremia as a sodium concentration below 135 mEq/L, generally caused by increased water retention. The types of hyponatremia are depletional and dilutional. Causes, symptoms, diagnostic workup and treatment approaches are described for hyponatremia. Hypernatremia is defined as a sodium level above 145 mEq/L. Causes, symptoms, and treatment focusing on calculating and correcting water deficit are covered for hypernatremia.
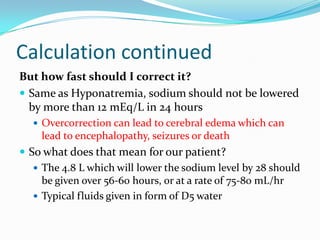
![Hypernatremia
Serum Na >145 mEq/L [deficit of (TBW)
relative to Na]
Incidence >1% in hospitalized patients.
Can have normal,hypo and hyperosmolality
Generally hypovolumic due to free water
loss , also hypervolumic is seen as itragenic
treatment with free accesses of water in
hospitals](https://image.slidesharecdn.com/hypo-hpernatrimia-130706220608-phpapp02/85/Hypo-hpernatrimia-33-320.jpg)
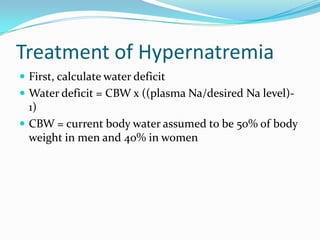
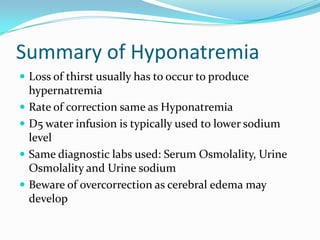
![•60 kg woman with 168 mEq/L
•How much water will it take to
reduce her sodium to 140 mEq/L
sample calculation:
Water deficit =
0.4 x 60 ([168/140]-1) = 4.8 L](https://image.slidesharecdn.com/hypo-hpernatrimia-130706220608-phpapp02/85/Hypo-hpernatrimia-39-320.jpg)