This document discusses sodium imbalance and hyponatremia. It provides details on:
- Normal sodium regulation and the causes of hyponatremia being related to water excess relative to sodium.
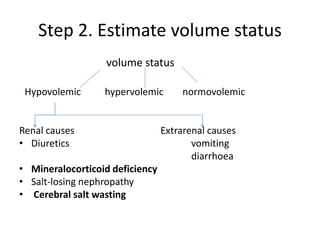
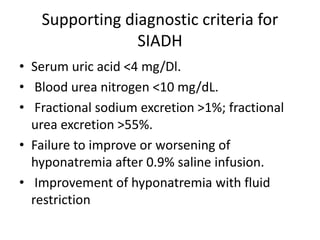
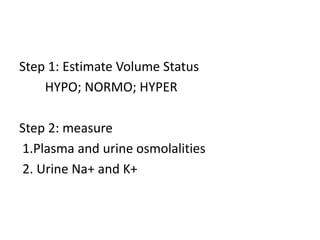
- The approach to evaluating hyponatremia by measuring osmolality, estimating volume status, and getting urinary sodium and osmolality levels.
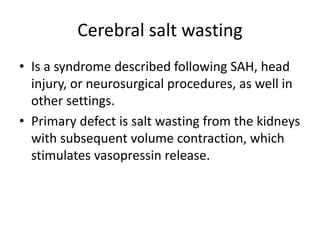
- Specific causes of hyponatremia like SIADH, cerebral salt wasting, and mineralocorticoid deficiency.
- The treatment of hyponatremia depending on if it is acute or chronic and correcting it slowly to avoid osmotic demyelination syndrome.
![SODIUM REGULATION
• Normal value: 135-145mEq/L.
• 85-90% sodium is extracellular.
• Sodium is responsible for more than 90%of total osmolality of
ECF.
• Major function is to maintain ECF volume and therefore
maintain blood pressure.
• Daily requirement is about 100mEq or 6gm of sodium
chloride.
• Excess salt is excreted chiefly by kidneys.
• Total body sodium is mainly regulated by aldosterone and
ANP.
• ADH, which is secreted in response to increased osmolality or
decreased blood pressure, primarily regulates [Na+]](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-2-320.jpg)











![• Equations : help calculate the initial rate of
fluids to be administered.
• A widely used formula is the Adrogue-Madias
formula.
• Change in serum Na+ with infusing solution=
infusate (Na + K)]-serum Na = [Na+] change by 1 liter of
infusate.
(total body water +1)](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-18-320.jpg)
![Treatment of Chronic Symptomatic
Hyponatremia
• For chronic hyponatremia, the plasma [Na]
should not rise faster than 0.5 mEq/L per hour
i.e. 10–12 mEq/L in 24 hours, and < 18 mEq in
48 hrs.
• Use 3 % NaCl, but Once symptoms and signs
improve, either water restriction or normal
saline should be started](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-19-320.jpg)
![Treatment of Asymptomatic
Hyponatremia
• In such patients, check volume status. For
hypovolemic patients, administration of
normal saline will improve both
hemodynamics and serum [Na+].
• FLUID EXCESS IS PRESENT.](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-20-320.jpg)
![• Fluid restriction required: the sum of urine
[Na+] and [K+] divided by serum [Na+] can be
used in the restriction of fluids/day.
Ratio Daily fluid intake (mL)
>1 <500
1 500 to 700
< 1 1000
simplest way to restrict fluids: input = output](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-21-320.jpg)

![Osmotic Demyelination Syndrome
• Previously called central pontine myelinolysis, is a
complication of treatment of hyponatremia.
• Due to rapid correction of chronic hyponatremia.
• When serum [Na+] is rapidly raised, the plasma
osmolality becomes hypertonic to the brain with
resultant water movement from the brain. This
cerebral dehydration probably causes
myelinolysis and ODS.](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-23-320.jpg)
![• Several risk factors for precipitation of OSD have
been identified. These are:
• 1. Chronic
• 2. Serum [Na+] < 105 mEq/L
• 3. Chronic alcoholism
• 4. Malnutrition
• 5. Hypokalemia
• 6. Severe liver disease
• 7. Elderly women on thiazide diuretics](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-24-320.jpg)

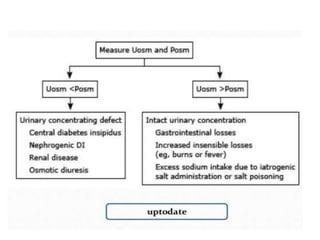
![HYPERNATREMIA
• Hypernatremia is defined as serum or plasma
[Na+] > 145 mEq/L
• Hypernatremia is seen in about 1% of
hospitalized patients and is more common
(7%) in intensive care unit patients.](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-26-320.jpg)









![• Free Water Replacement: The calculation of
free water deficit
• Current TBW = Normal TBW × (140/Current
[PNa])
• H2O Deficit (L) = Normal TBW – Current TBW
= TBW ( 1 – 140/ Current NA)](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-38-320.jpg)
![• REPLACEMENT VOLUME: Free water deficits
are corrected with sodium-containing fluids
such as 0.45% NaCL
• Volume (L) = H2O Deficit × (140/[Na] in IV
Fluid)](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-39-320.jpg)
![• RATE OF REPLA CEMENT:
1. aggressive replacement of free water deficits
can produce cell swelling and cerebral edema.
2. the decrease in plasma [Na+] should not exceed
0.5 mEq/L per hour during free water
replacement
3. time needed to reduce the plasma [Na+] to 140
mEq/L at a rate of 0.5 mEq/L/hr is
Actual Na – 140
0.5](https://image.slidesharecdn.com/sodiumimbalance-181110053345/85/Sodium-imbalance-40-320.jpg)