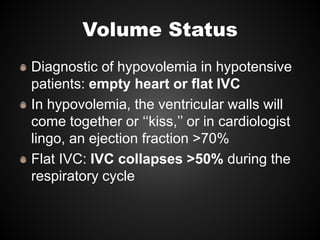
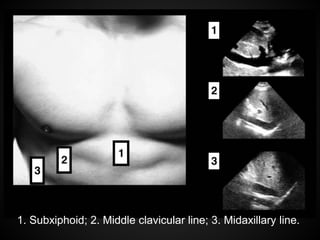
Point-of-care cardiac ultrasound, also known as focused cardiac ultrasound (FoCUS), can be performed at the bedside by any treating clinician to evaluate hypotensive patients. It uses 2D ultrasound to visualize the heart's size, function and anatomy without advanced training or technology. FoCUS can differentiate shock types and guide fluid resuscitation by examining the heart, lungs and IVC for signs of volume status. A normal, collapsing IVC suggests hypovolemia while B-lines in the lungs discourage further fluids for possible edema. RV size helps diagnose pulmonary embolism. This review discusses the clinical applications and techniques of FoCUS to rapidly diagnose and treat unstable patients.