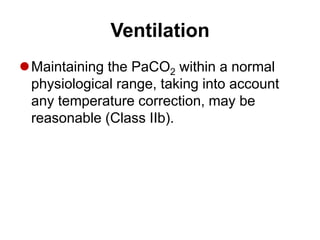
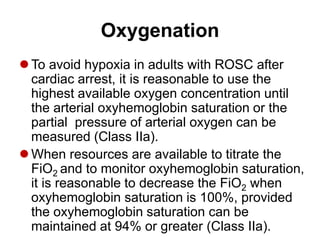
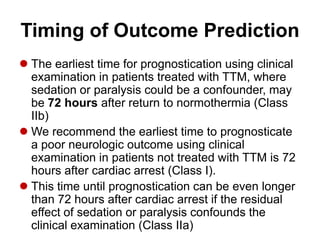
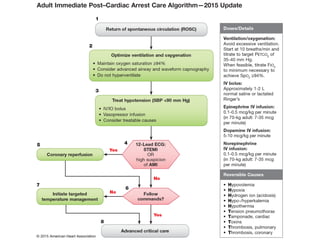
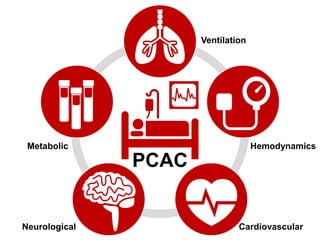
This document provides guidelines for post-cardiac arrest care. It recommends:
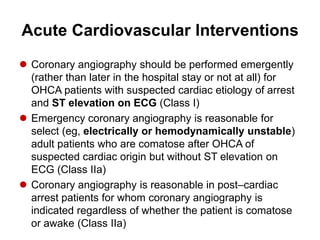
1) Performing emergency coronary angiography for OHCA patients with suspected cardiac cause and ST elevation on ECG.
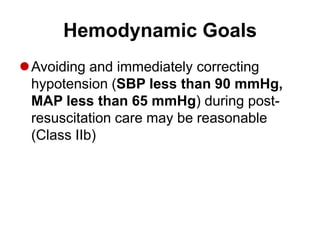
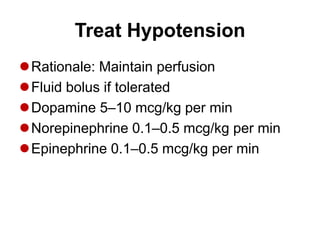
2) Maintaining blood pressure above 90 mmHg systolic or 65 mmHg mean and immediately correcting any hypotension.
3) Inducing therapeutic hypothermia between 32-36°C for at least 24 hours in comatose cardiac arrest patients to minimize brain injury.
![Post–Cardiac Arrest Care
Circulation. 2015;132[suppl 1]:S465–S482.](https://image.slidesharecdn.com/postcardiacarrestcare-151229025455/85/Post-Cardiac-Arrest-Care-1-320.jpg)