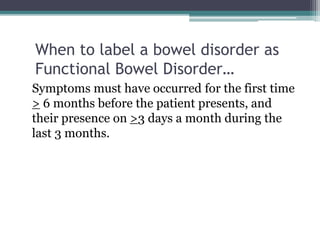
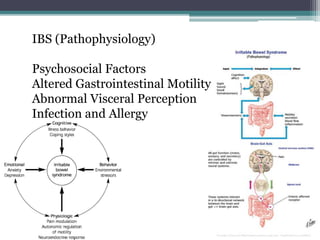
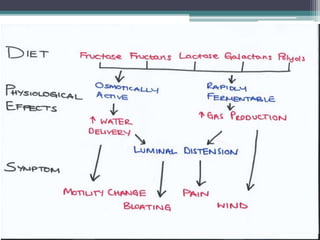
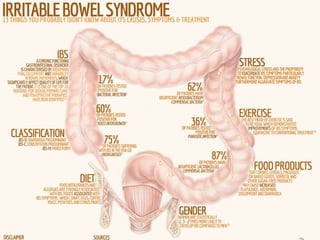
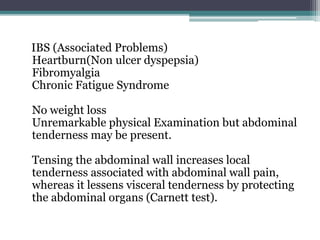
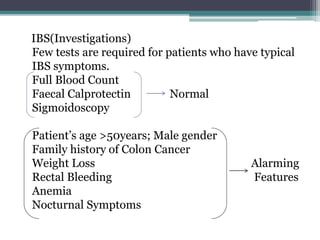
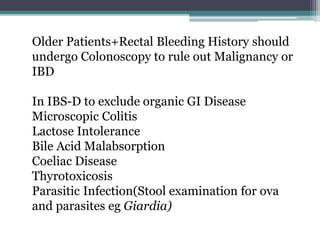
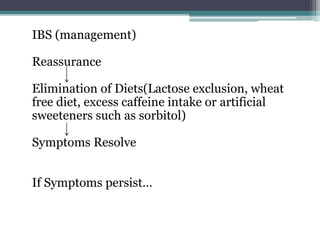
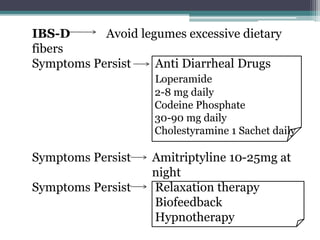
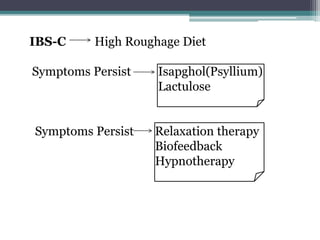
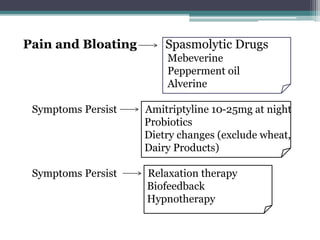
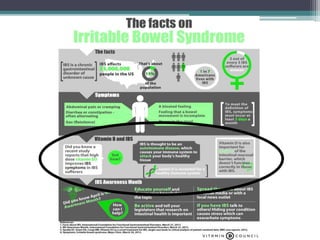
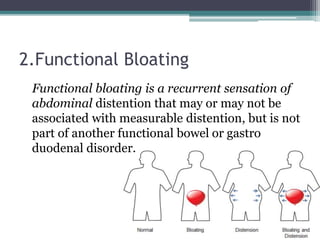
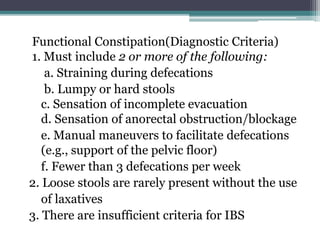
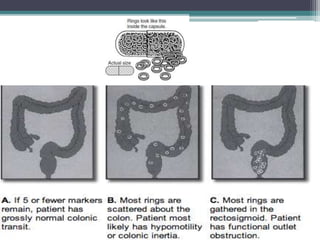
This document defines and classifies functional bowel disorders, including irritable bowel syndrome (IBS), functional constipation, functional diarrhea, and unspecified functional bowel disorders. IBS is further described in terms of pathophysiology, clinical features, diagnostic criteria, subtypes, diagnosis supporting features, associated problems, investigations, and management approaches. Functional constipation and diarrhea are also defined and their diagnostic criteria, clinical evaluation, and treatment are outlined.