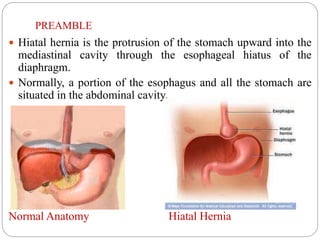
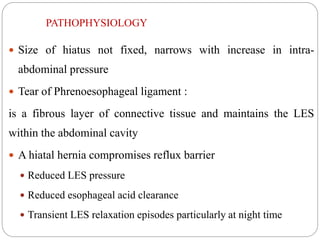
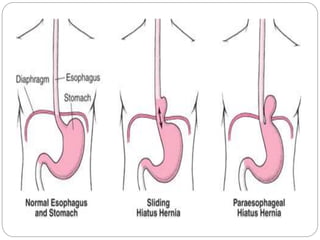
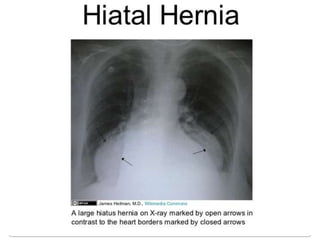
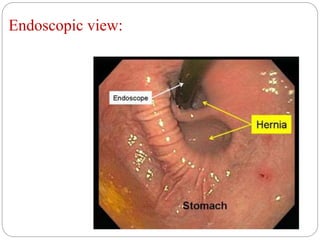
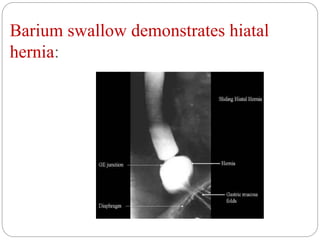
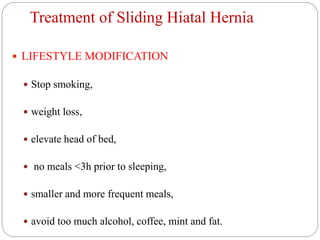
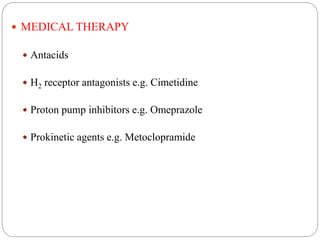
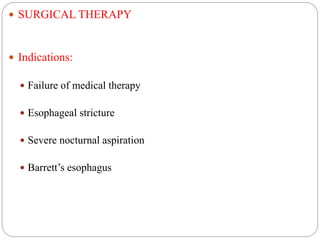
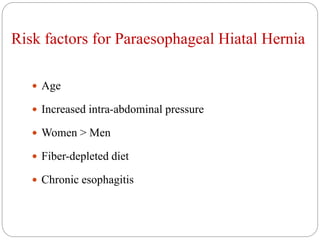
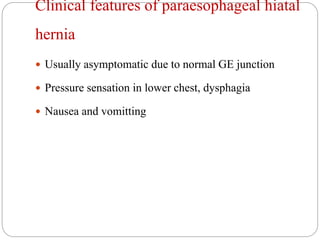
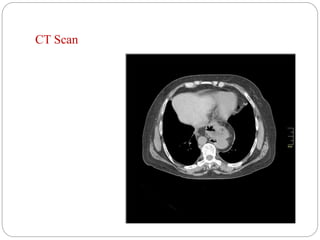
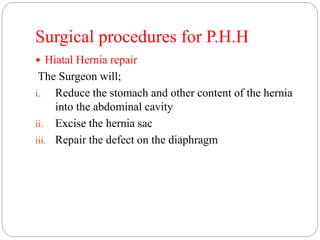
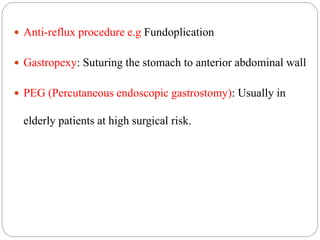
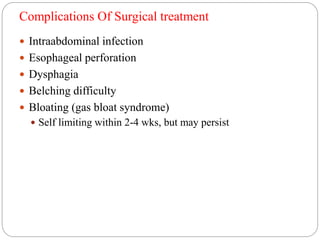
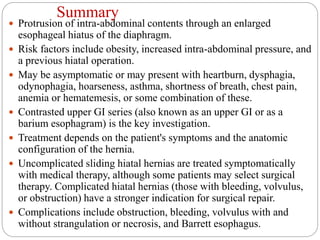
Hiatal hernia is a condition where the stomach and other intra-abdominal contents protrude through the esophageal hiatus of the diaphragm. Risk factors include obesity, increased abdominal pressure, and previous hiatal hernia surgery. Symptoms may include heartburn, dysphagia, chest pain, or respiratory issues. Diagnosis is typically made through upper gastrointestinal imaging. Treatment depends on symptoms and hernia type but may involve lifestyle changes, medication, or surgery to repair the diaphragmatic defect and prevent acid reflux. Complications can include obstruction, bleeding, stomach twisting, and Barrett's esophagus.
![References
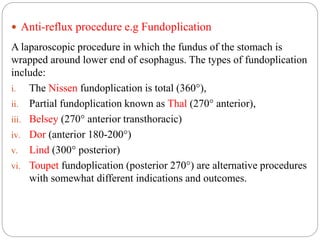
Renee C. Minjarez, M.D. and Blair A. Jobe, M.D. (2006).
"[Surgical therapy for gastroesophageal reflux disease.]". GI
Motility online
http://emedicine.medscape.com/article/178393-overview.
Retrieved on 22nd February, 2016
https://en.wikipedia.org/wiki/Esophageal_hiatus. Retrieved on
22nd February, 2016
Hall, J. and Premji, A (2015). The Toronto notes 2015:
Comprehensive medical reference and review for the Medical
Council of Canada Qualifying Exam Part 1 and the United
States Medical Licensing Exam Step 2. Toronto: Toronto Notes
for Medical Students, Inc.](https://image.slidesharecdn.com/hiatalhernia-160311101345/85/Hiatal-hernia-29-320.jpg)
