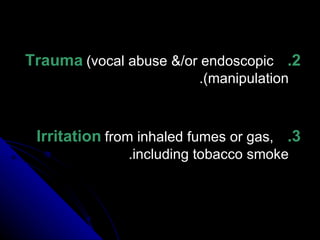
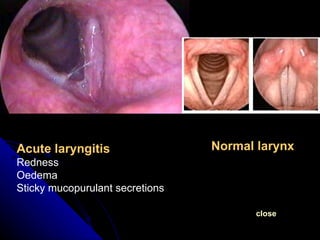
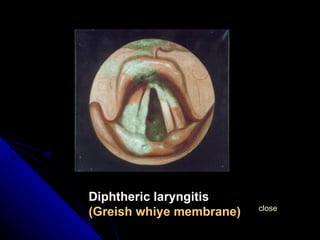
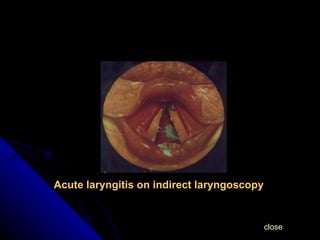
1. Acute laryngitis is swelling of the laryngeal mucosa and underlying tissue that is commonly caused by viral or bacterial infections, exogenous agents, or autoimmune processes.
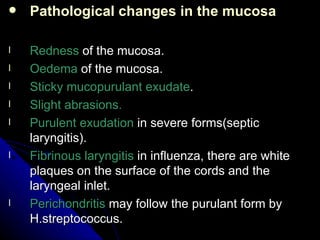
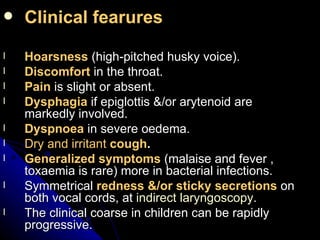
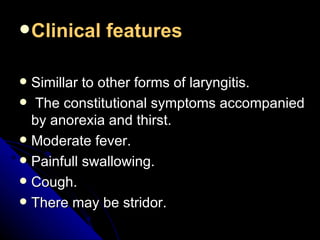
2. Symptoms include hoarseness, discomfort in the throat, dry cough, and dyspnea in severe cases. Examination may reveal redness and sticky secretions on the vocal cords.
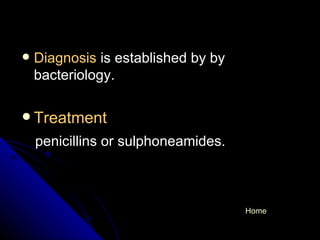
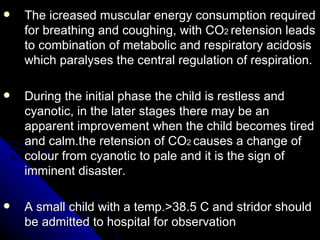
3. Treatment focuses on rest, steam inhalations, medications to reduce swelling and loosen secretions, and antibiotics for bacterial infections. Children require close monitoring due to risk of airway obstruction.