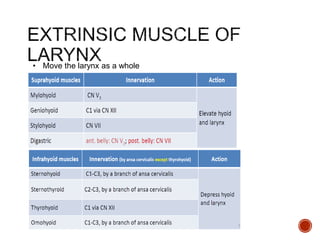
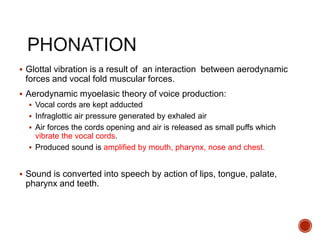
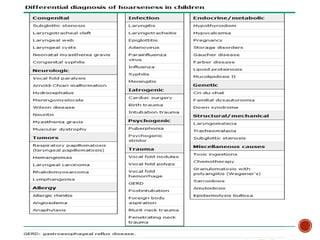
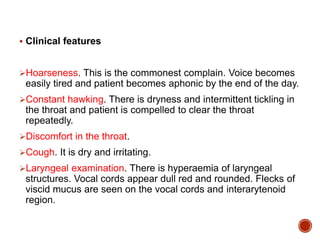
The document describes the anatomy and physiology of the larynx. It discusses the cartilages that make up the larynx, including the thyroid, cricoid, and epiglottis cartilages. It also describes the intrinsic and extrinsic membranes of the larynx. Furthermore, it discusses the functions of the larynx in phonation, respiration, and protection of the lower airways. It outlines common laryngeal pathologies like laryngitis and their causes, symptoms, and treatments.















































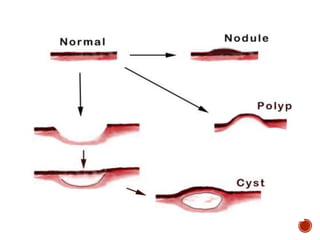




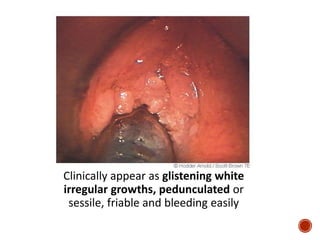
![ Postulated to be vertically transmitted during the process of
childbirth.
Almost all papillomas in the throat are caused by
HPV subtypes [HPV- 6, HPV-11, HPV-16 & HPV-18]. These same
subtypes that appear in the cervix.
Researchers believe that the throat can be infected during
childbirth passage through the cervix or from oral-genital sexual
activities.](https://image.slidesharecdn.com/hoarseness-year-4-160221235949/85/Hoarseness-year-4-58-320.jpg)