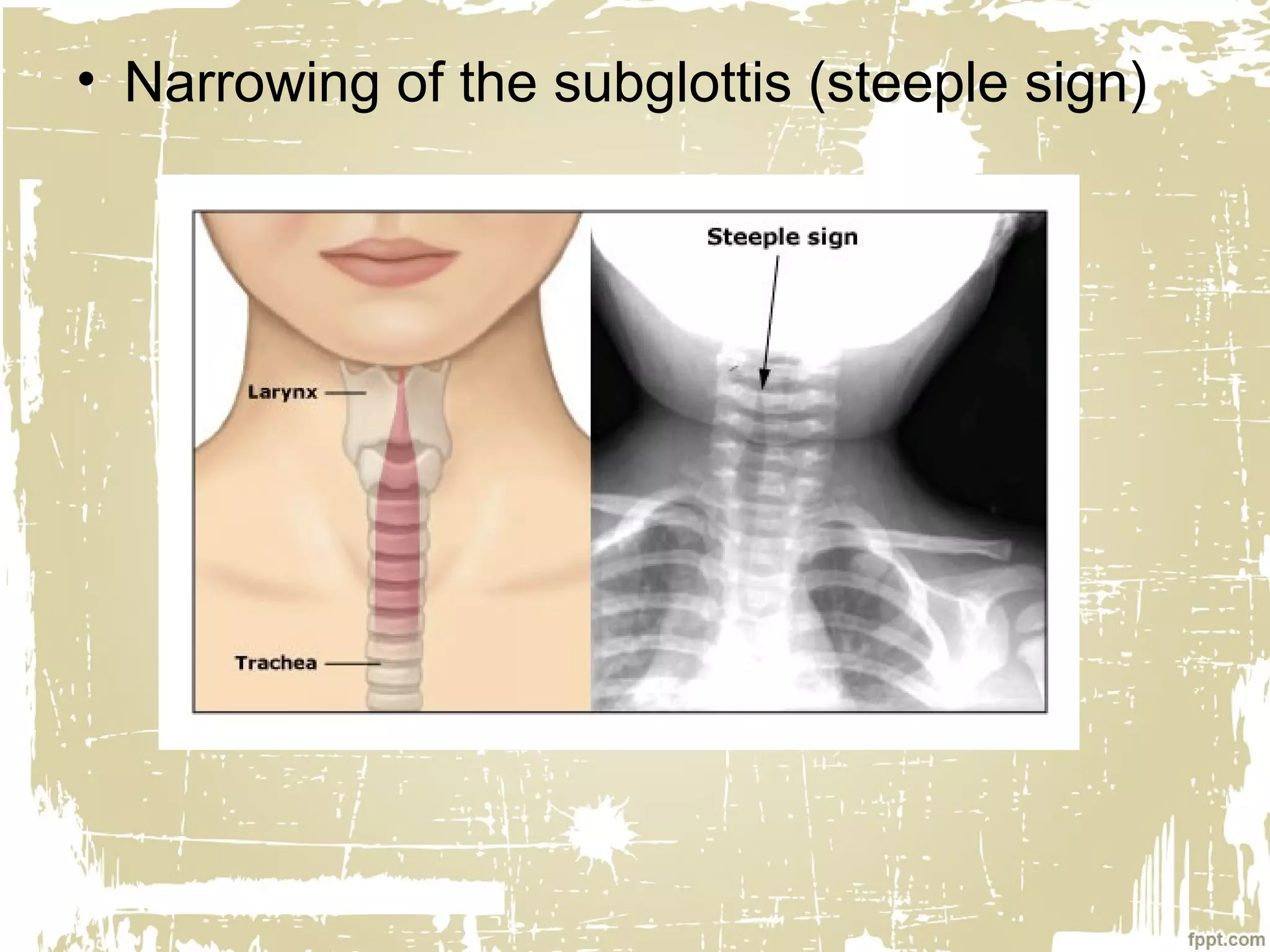
This document discusses laryngeal infections. It begins by introducing laryngitis as an inflammation of the larynx that can be acute or chronic. Acute laryngitis is usually self-limited while chronic lasts over 3 weeks. Causes include vocal misuse, noxious agents, and viruses or bacteria. In children, important acute laryngeal infections are epiglottitis, croup, and bacterial laryngotracheobronchitis. Chronic laryngitis can be caused by repeated acute infections or long-term irritants like smoking. Diagnosis involves examination and investigations depend on the suspected infection. Management involves treating the underlying cause, antibiotics, corticosteroids, and occasionally intubation or tracheostomy