This document discusses various types of acute and chronic laryngitis including:
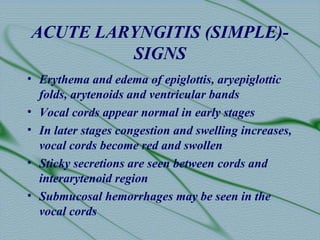
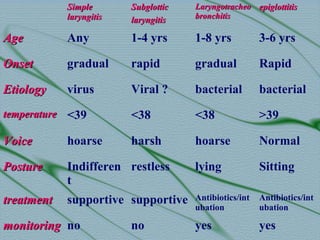
- Acute laryngitis (simple laryngitis), which is usually caused by viral infections and results in inflammation of the larynx. Symptoms include hoarseness and treatment focuses on vocal rest and antibiotics.
- Acute fibrinous laryngitis, which mainly affects young children and involves inflammation of the entire respiratory tract. It can cause respiratory obstruction.
- Subglottic laryngitis, which presents with croup-like symptoms in young children without fever.
- Acute epiglottitis, which is a medical emergency caused by bacterial infection and seen more commonly in children. Symptoms include sore