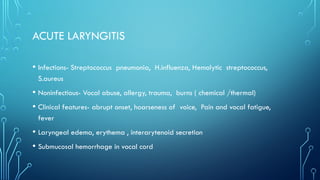
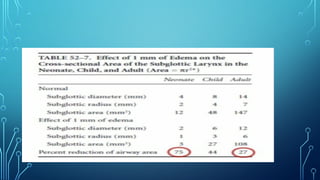
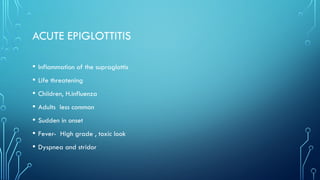
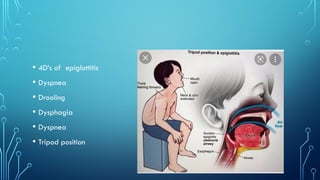
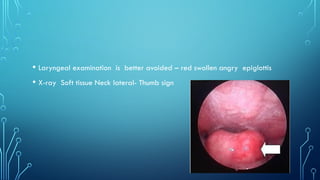
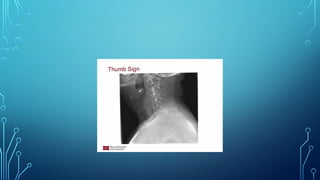
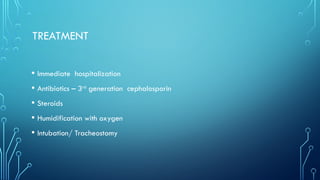
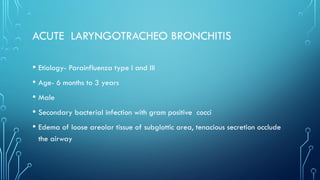
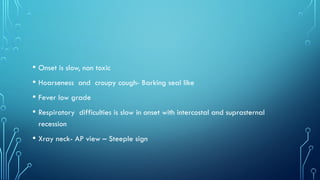
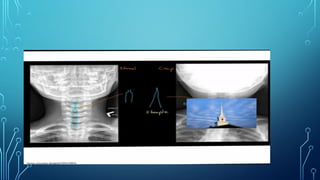
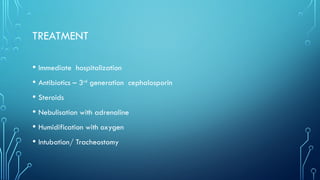
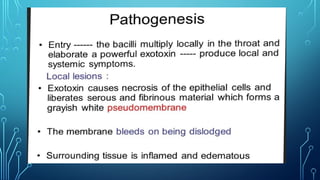
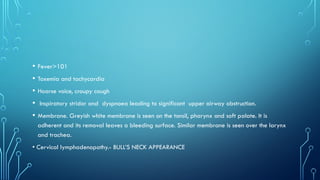
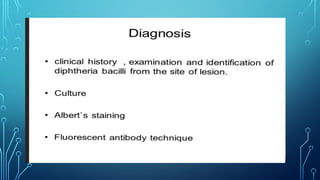
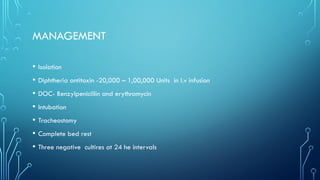
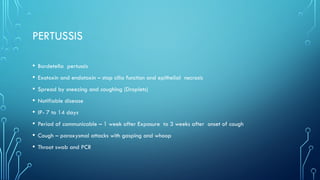
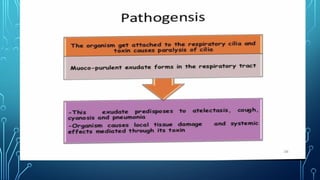
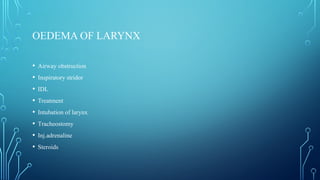
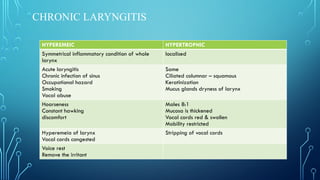
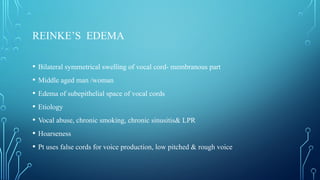
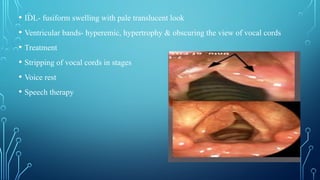
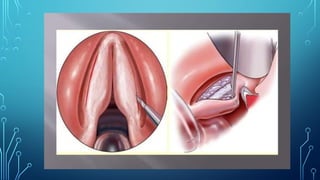
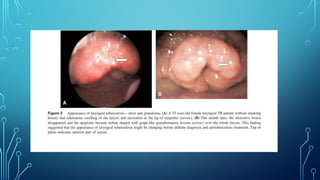
The document discusses various conditions affecting the larynx, including acute and chronic laryngitis, epiglottitis, laryngotracheobronchitis, and laryngeal diphtheria, outlining their causes, clinical features, and management strategies. It highlights the significance of timely diagnosis and treatment to prevent complications like airway obstruction and asphyxia. Management approaches include voice rest, antibiotics, steroids, and surgical interventions as needed.