Here are the definitions and explanation requested:
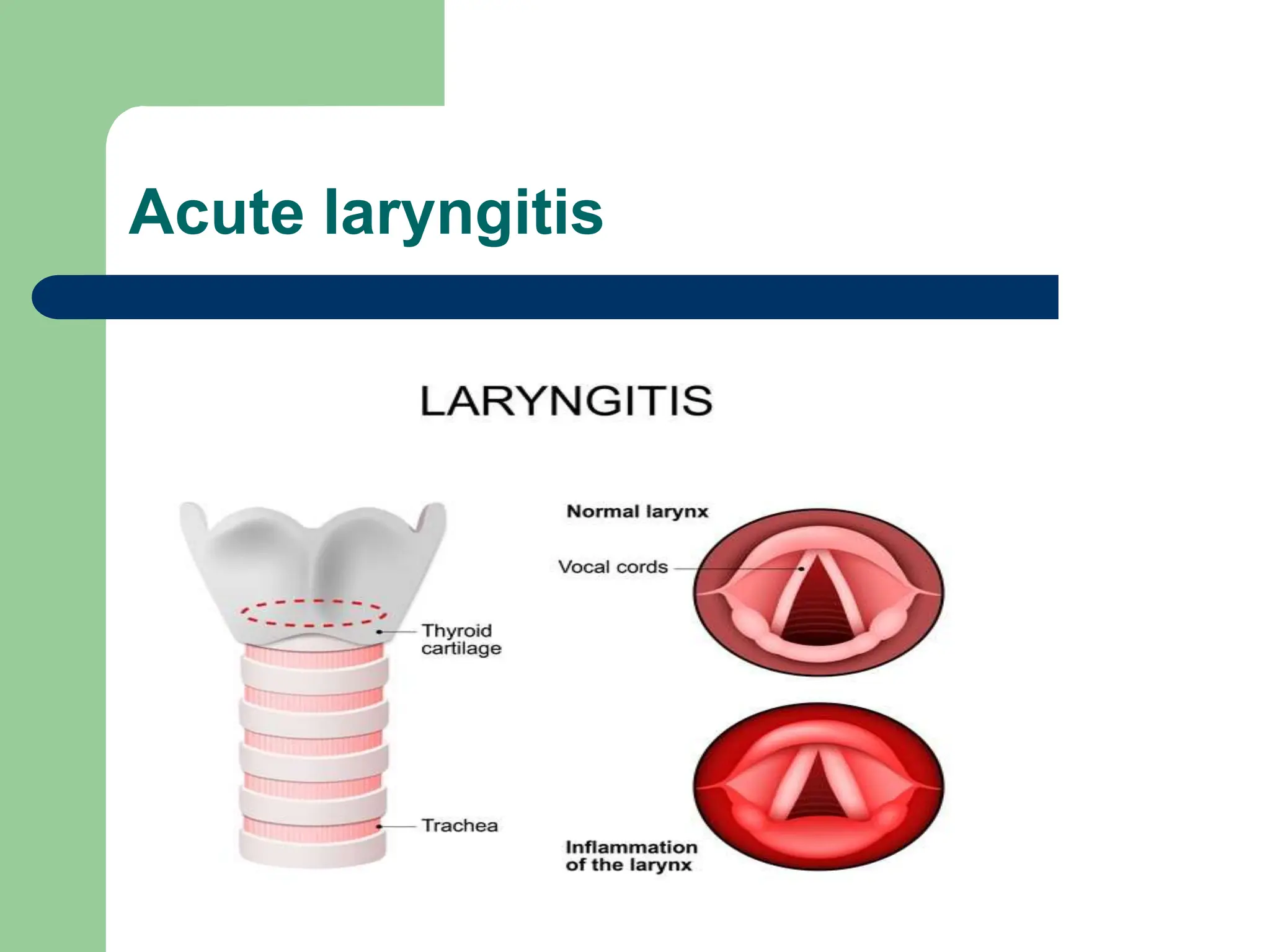
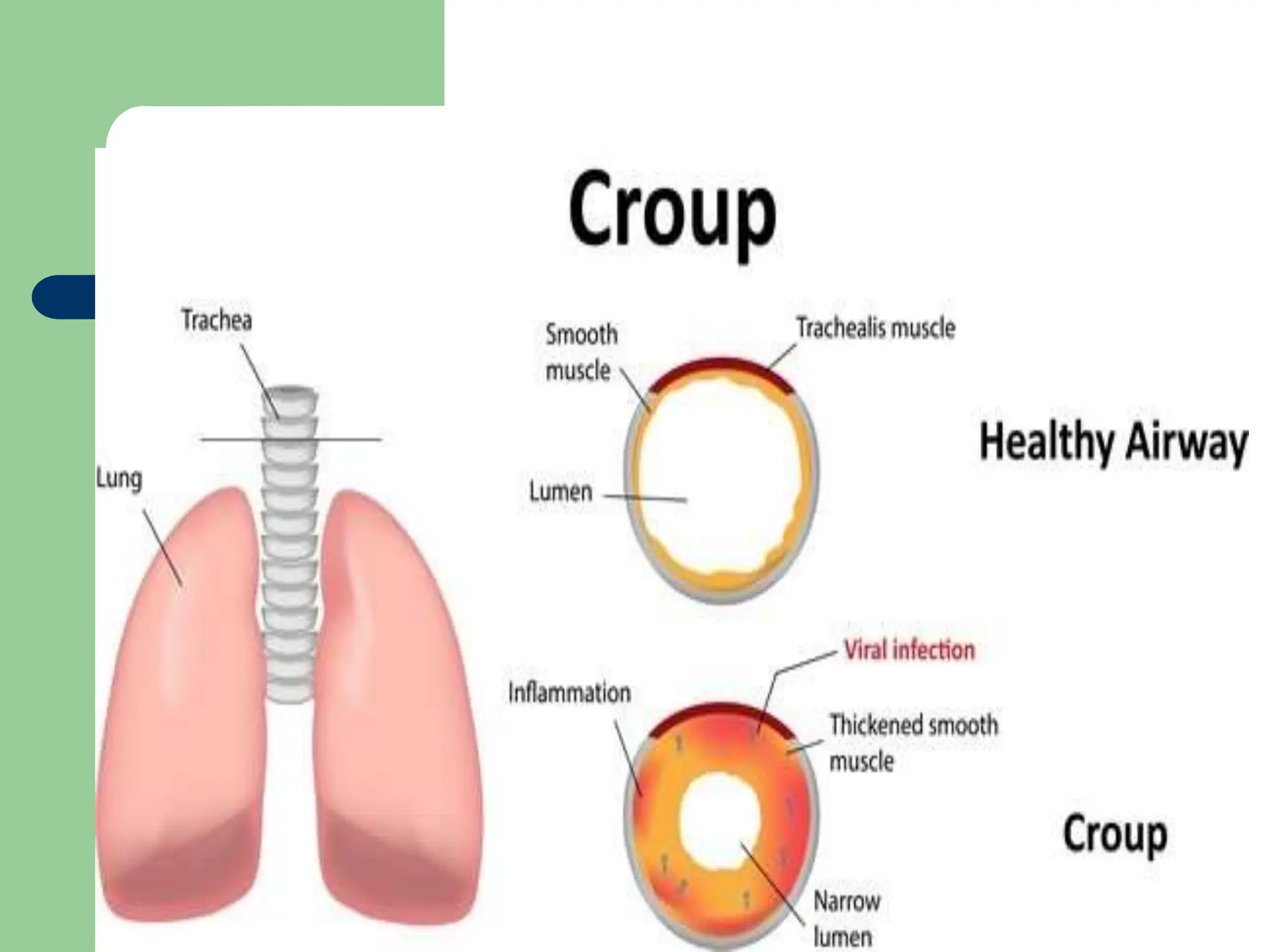
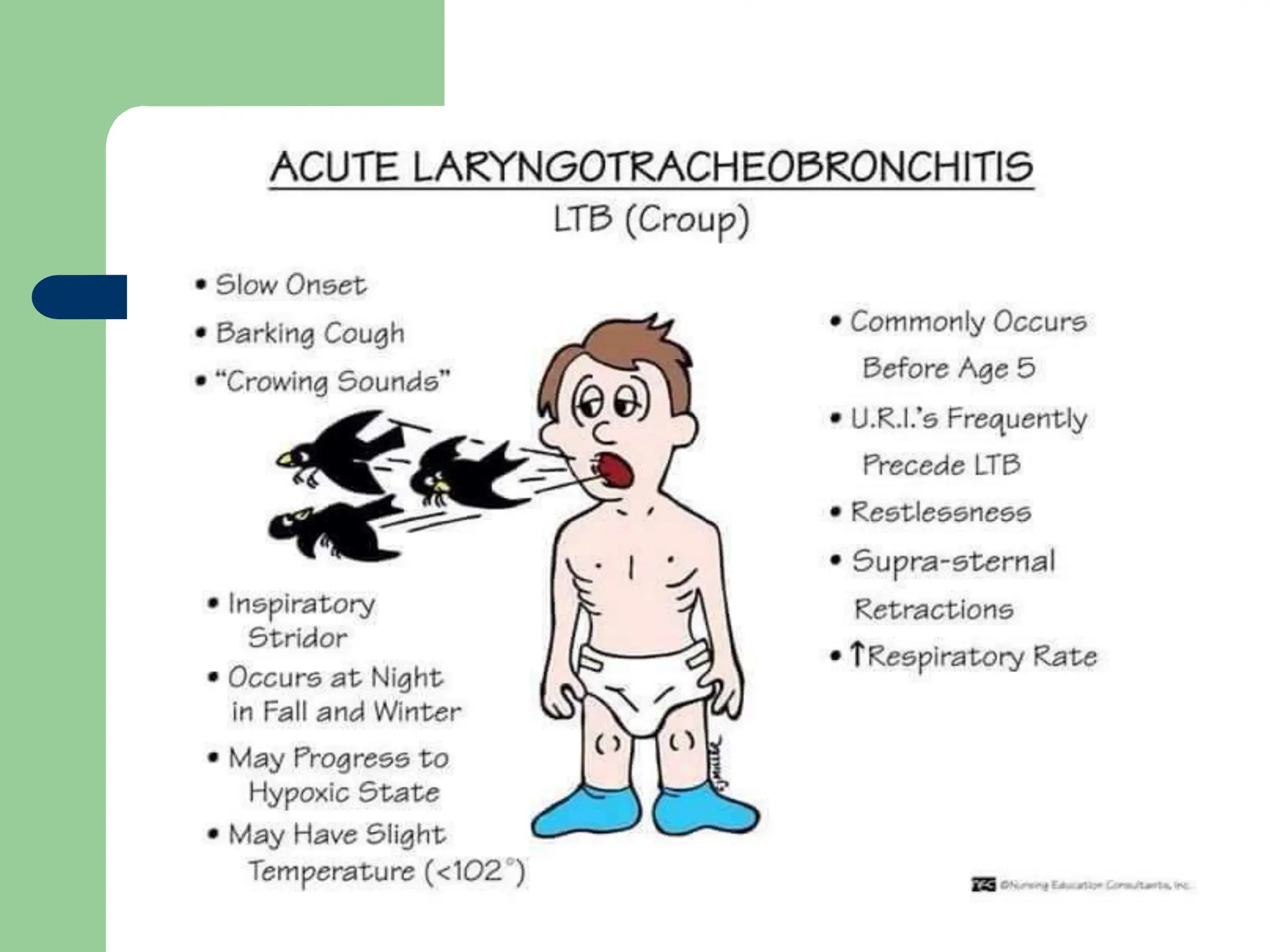
Croup syndrome is a respiratory illness characterized by inspiratory stridor, cough, and hoarseness caused by inflammation and obstruction of the larynx, trachea, and major bronchi.
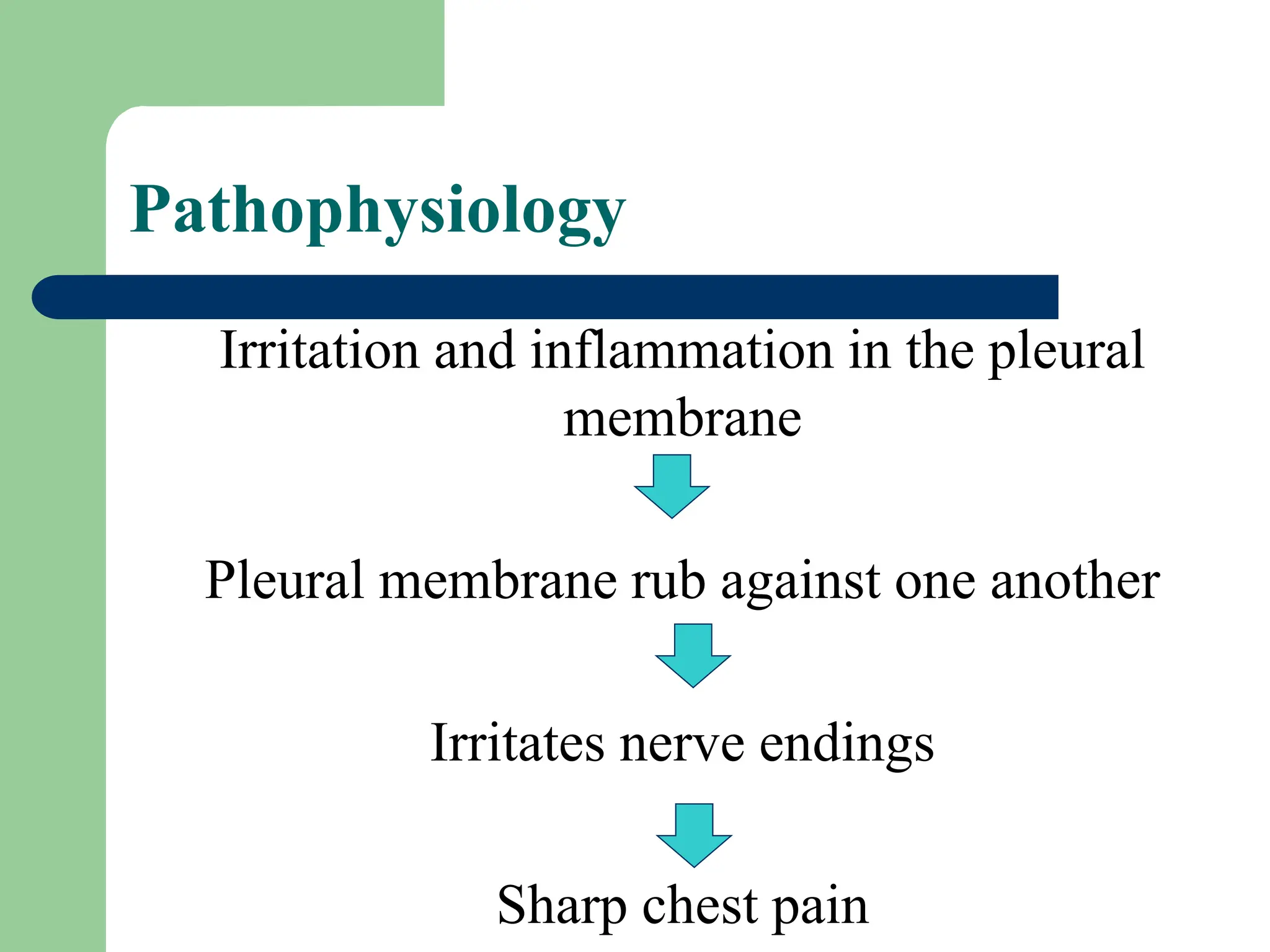
Pleurisy is defined as inflammation of the pleura, the thin membrane that lines the chest cavity and covers the lungs. It is also called pleuritis.
The causes of pleurisy include:
- Respiratory infections like pneumonia, tuberculosis, and other bacterial or viral infections that can cause inflammation of the pleura.
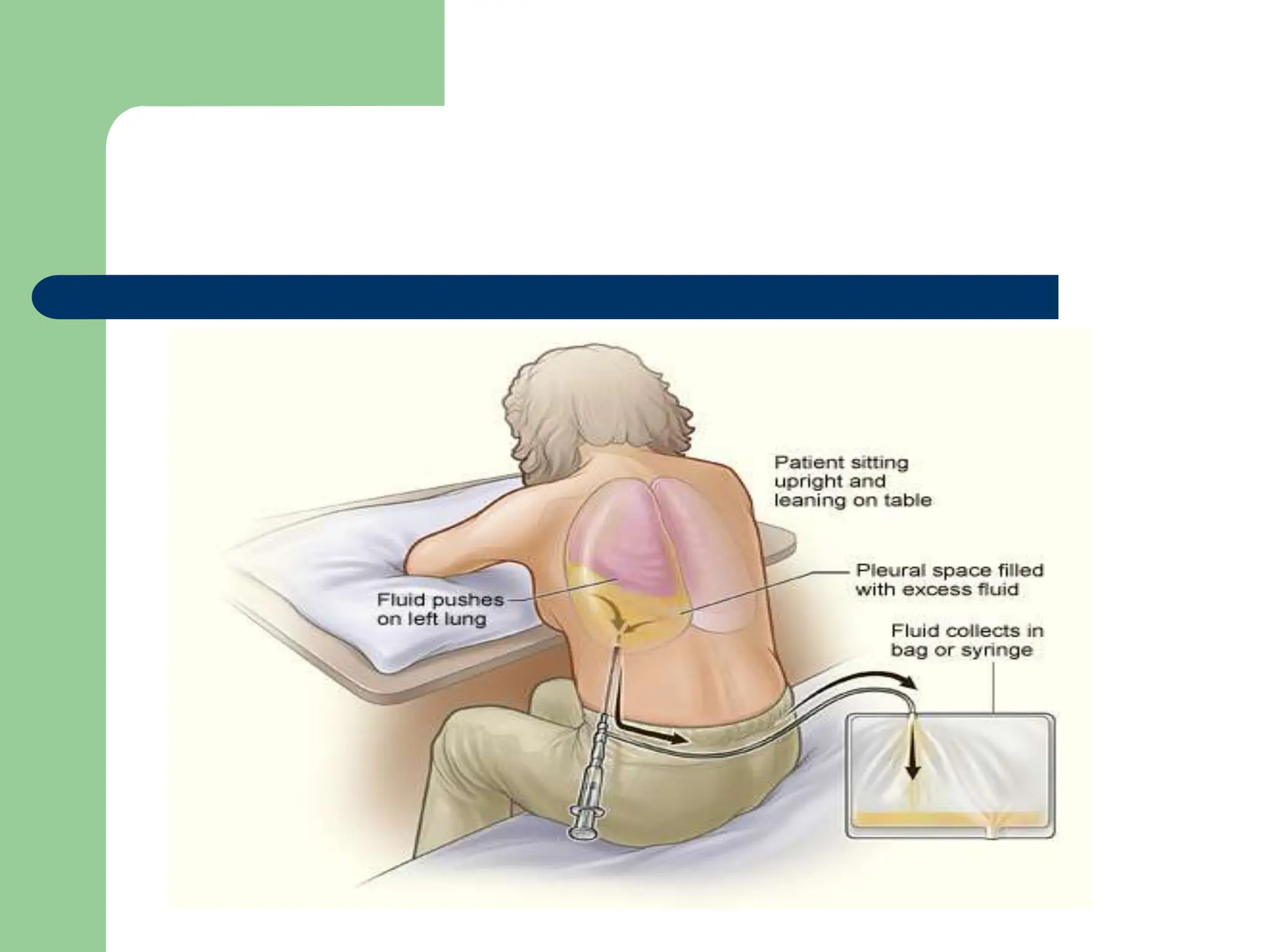
- Immune disorders such as systemic lupus erythematosus and rheumatoid arthritis where excess fluid builds up in the pleural space