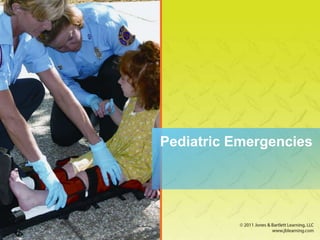
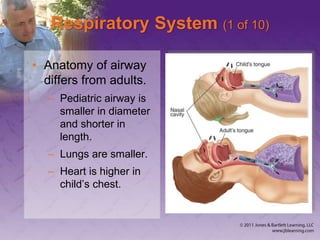
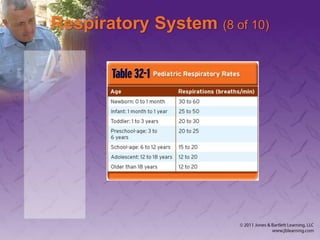
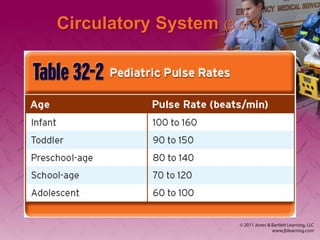
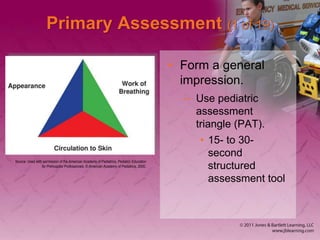
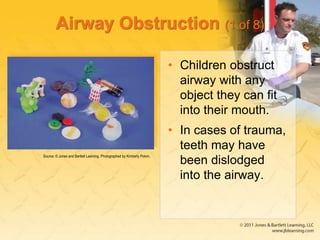
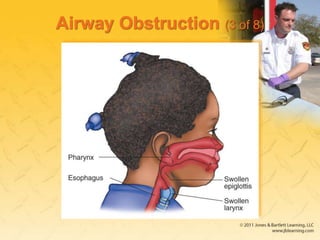
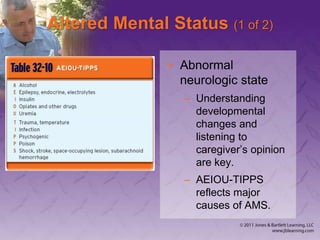
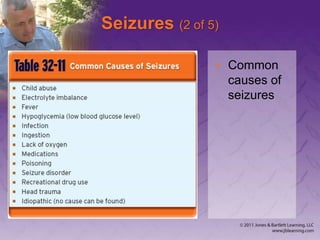
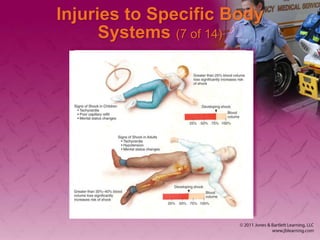
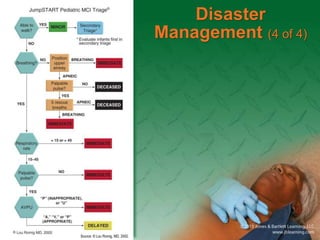
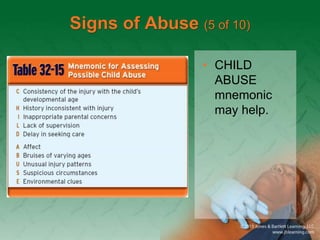
This document outlines pediatric emergency competencies for EMS providers, including respiratory emergencies like airway obstruction, lower airway disease, and respiratory distress; shock; seizures; and sudden infant death syndrome. It also covers patient assessment procedures, respiratory system anatomy, circulatory system overview, respiratory and airway emergency management, shock treatment, altered mental status causes, seizure first aid, dehydration treatment, fever reduction, injury management, disaster triage, signs of child abuse and neglect, and details on sudden infant death syndrome.