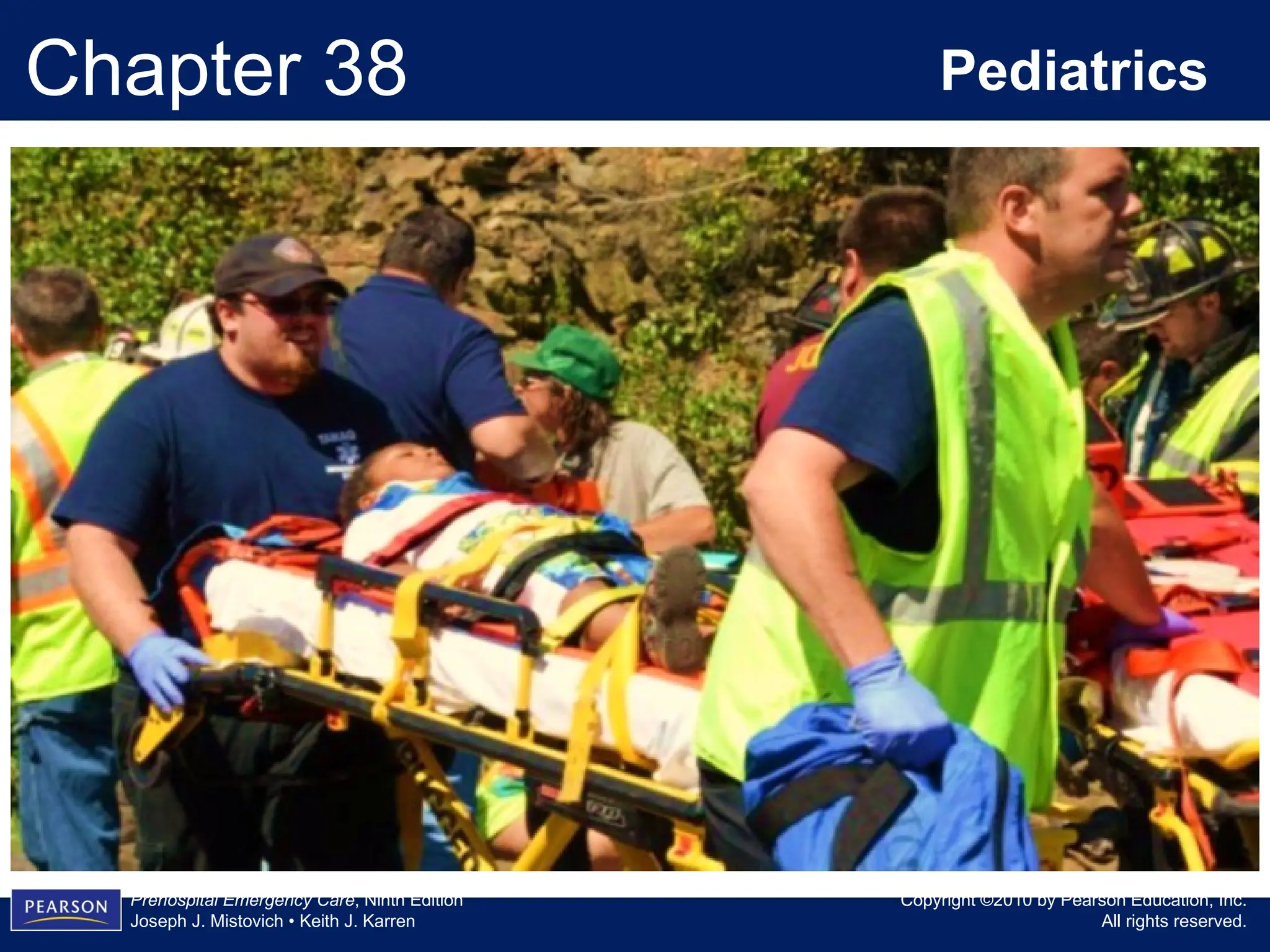
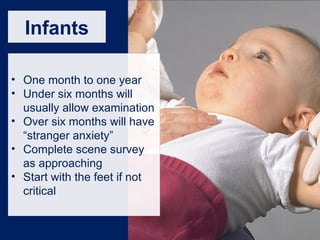
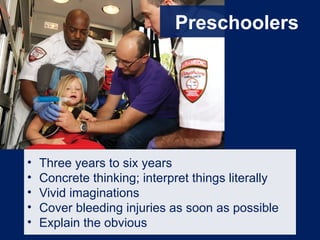
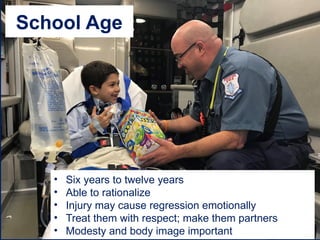
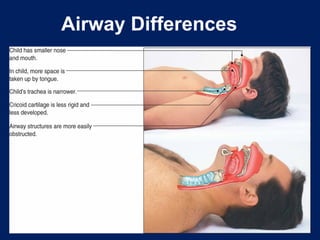
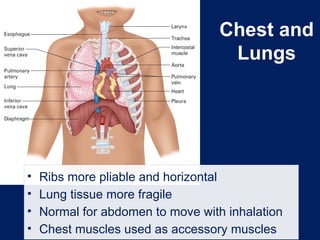
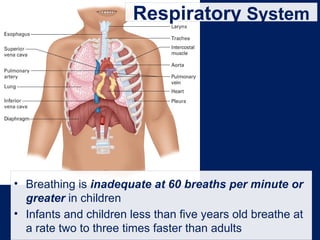
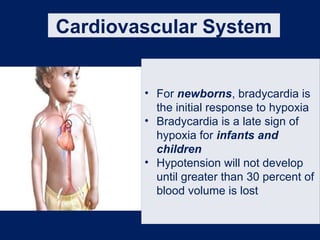
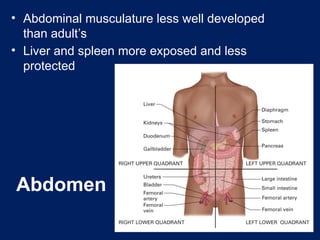
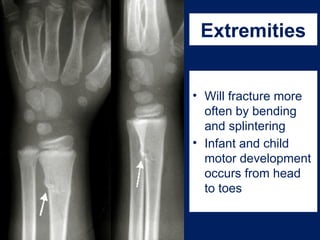
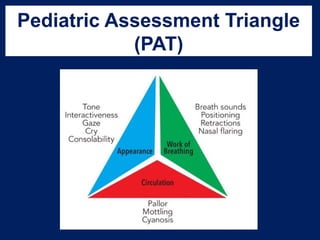
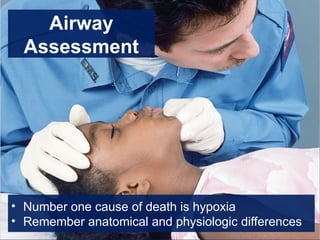
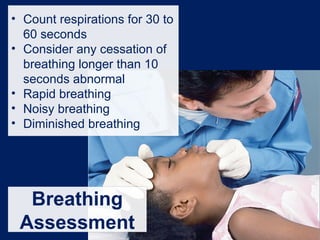
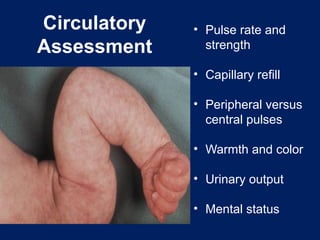
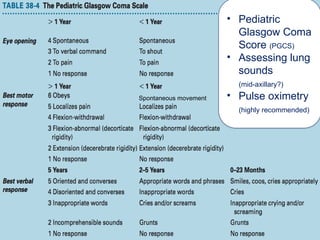
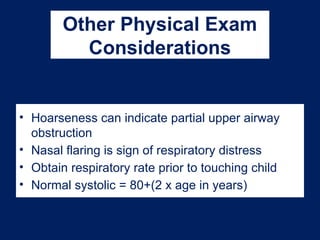
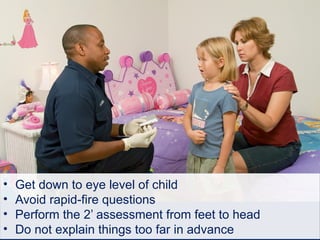
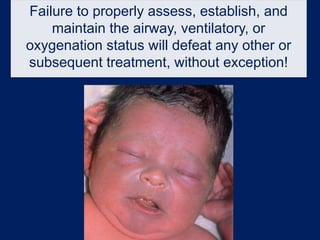
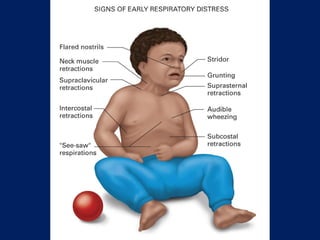
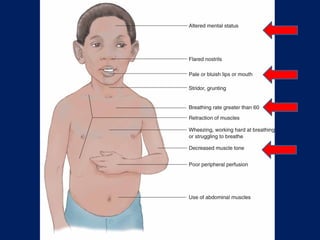
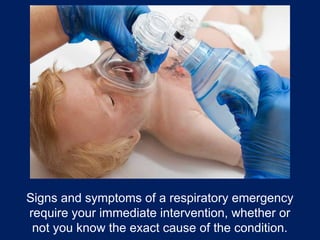
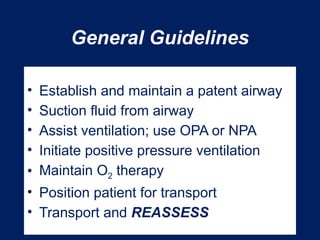
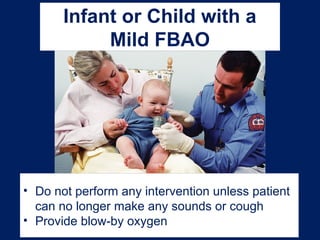
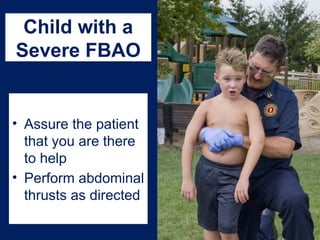
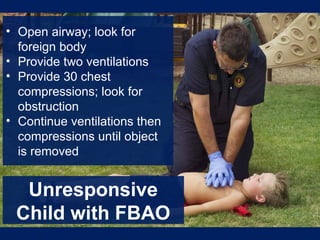
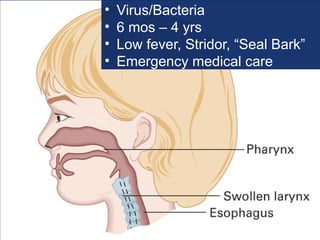
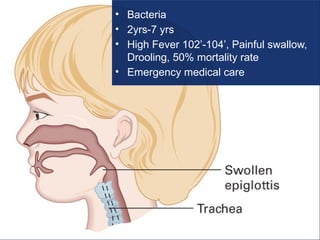
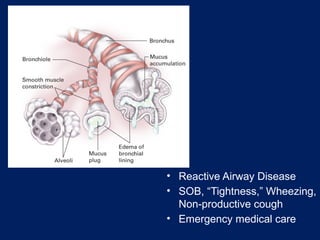
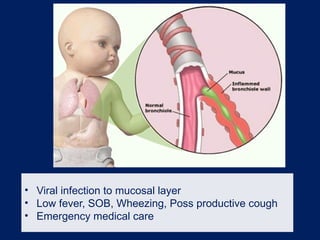
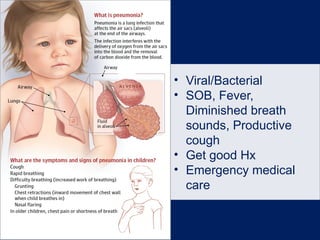
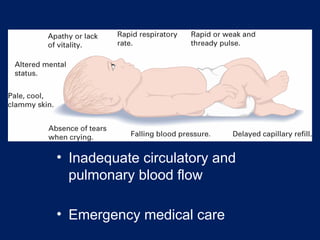
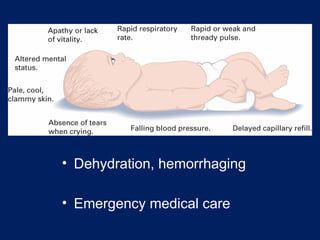
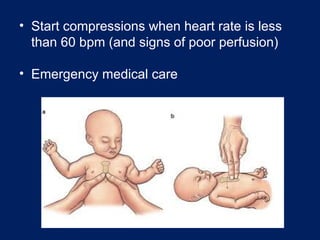
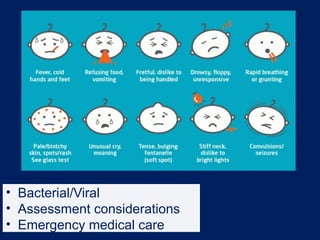
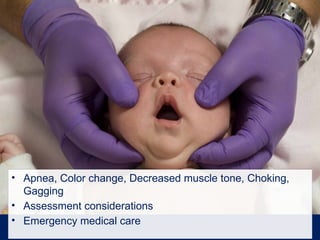
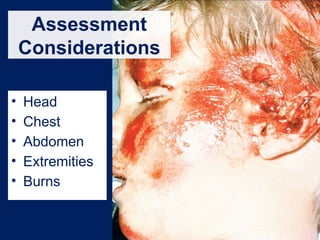
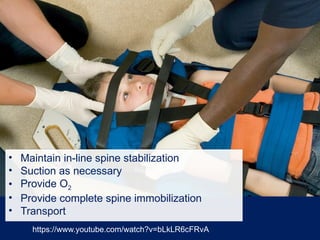
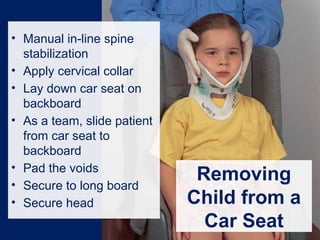
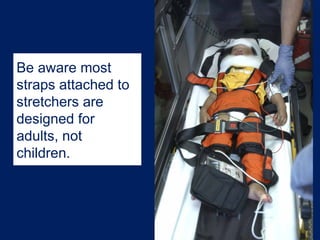
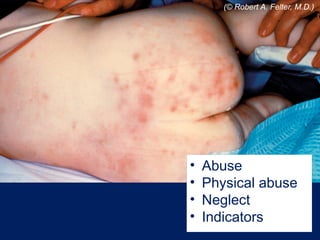
The document provides comprehensive guidelines for pediatric emergency care, highlighting developmental characteristics, assessment techniques, and special considerations for various age groups from neonates to adolescents. It outlines critical differences in anatomy, physiology, and common emergent conditions, emphasizing the importance of establishing and maintaining a patent airway and recognizing the signs of respiratory and cardiopulmonary issues. Additionally, it discusses trauma management, injury prevention, and care for children with special health care needs, reinforcing a family-centered approach.