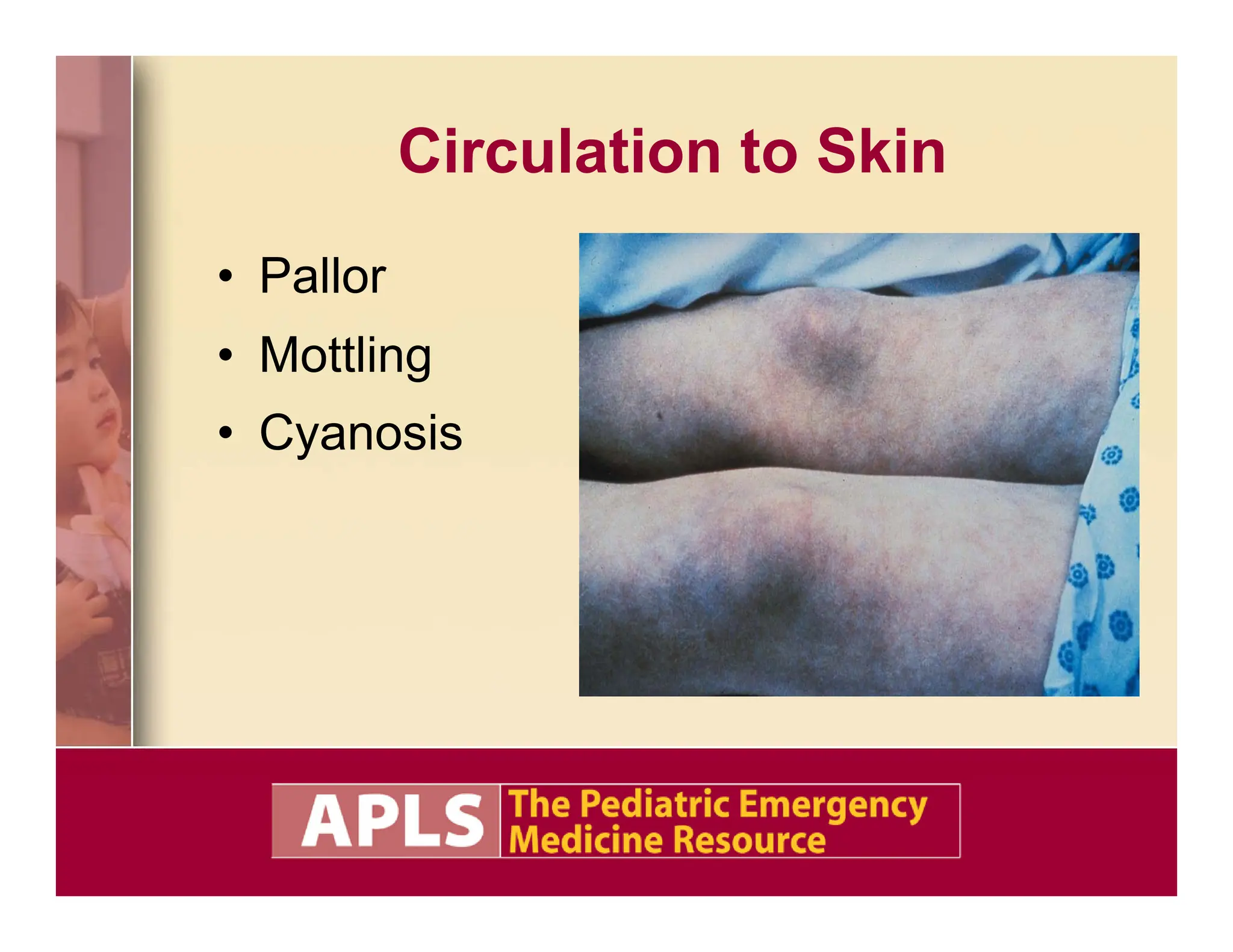
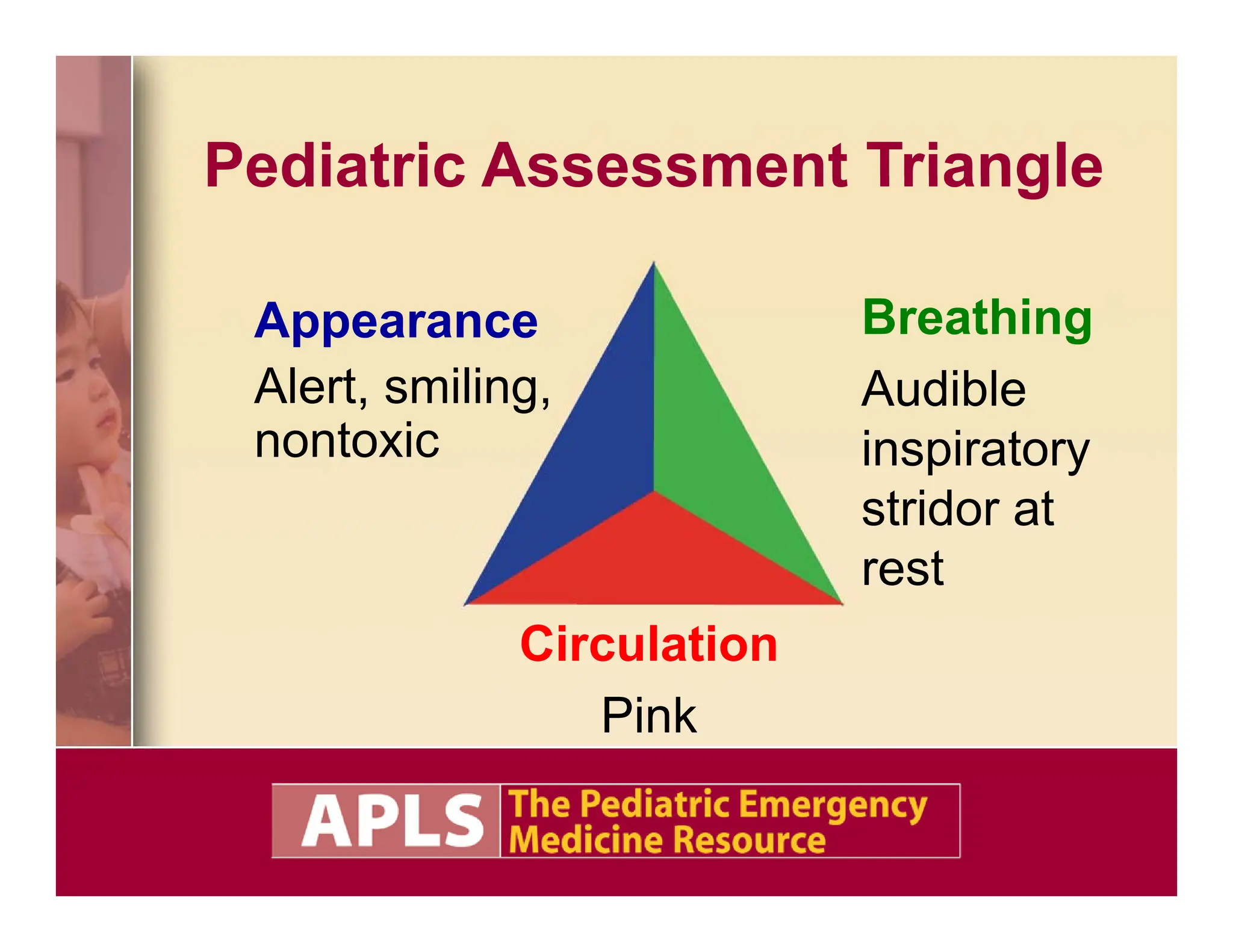
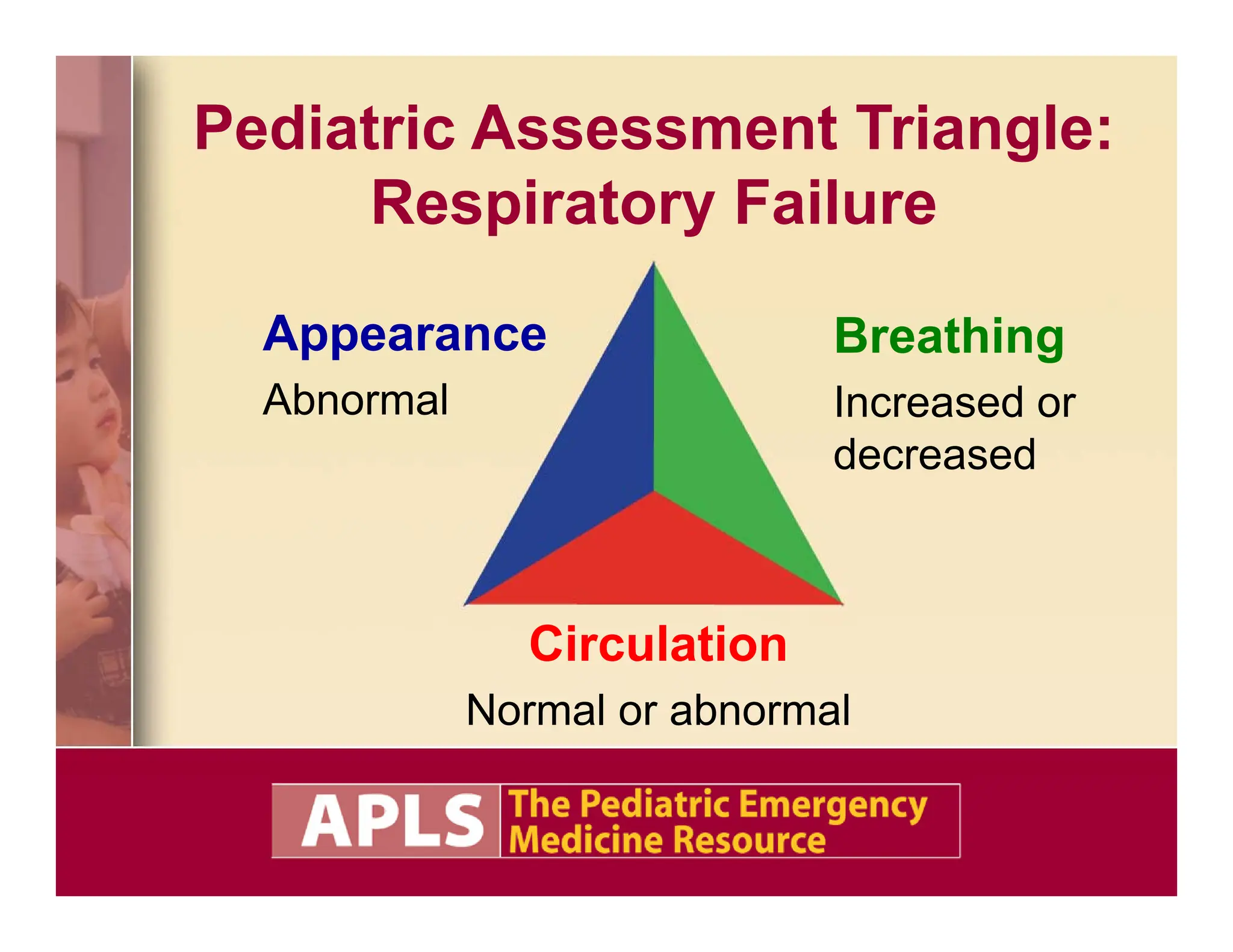
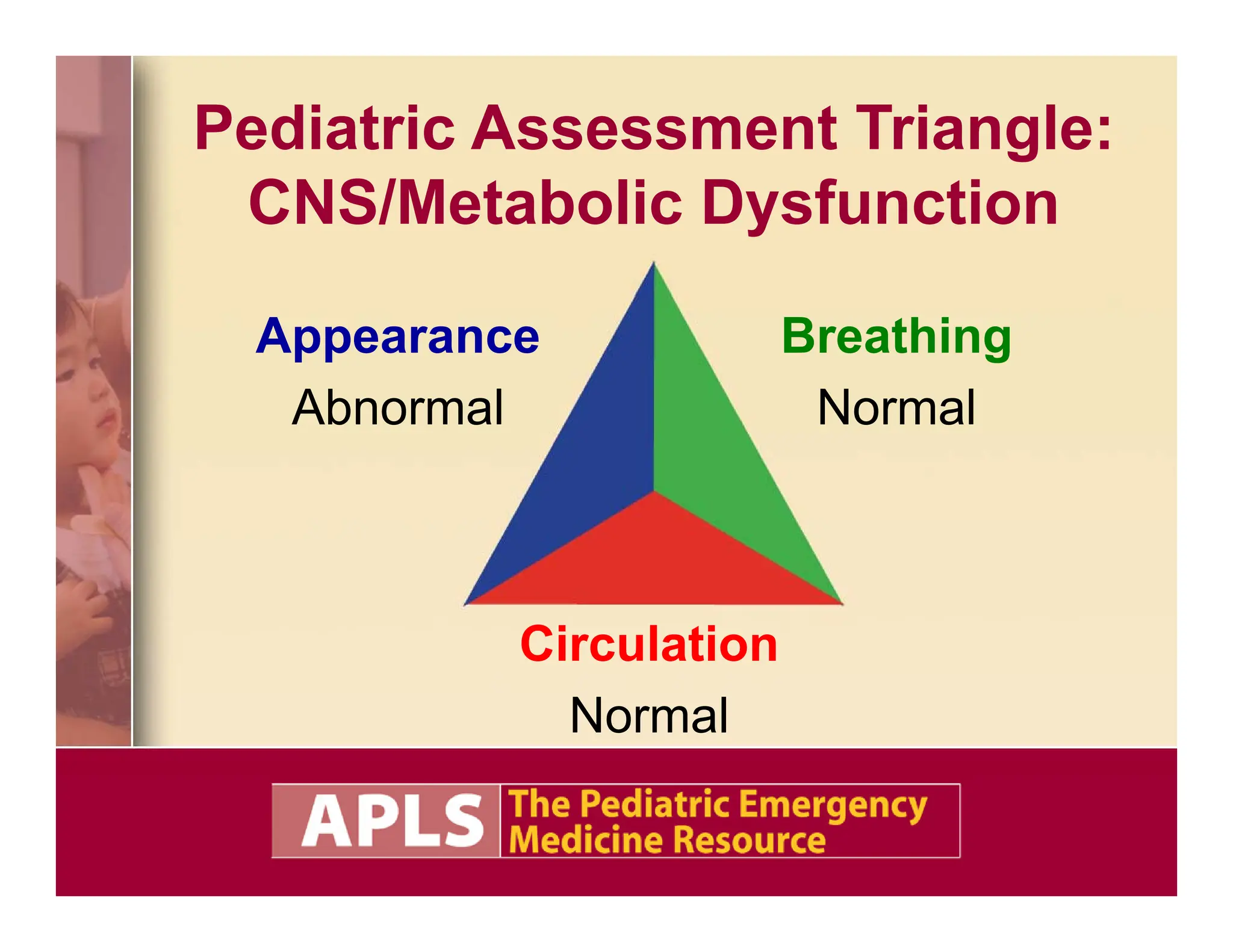
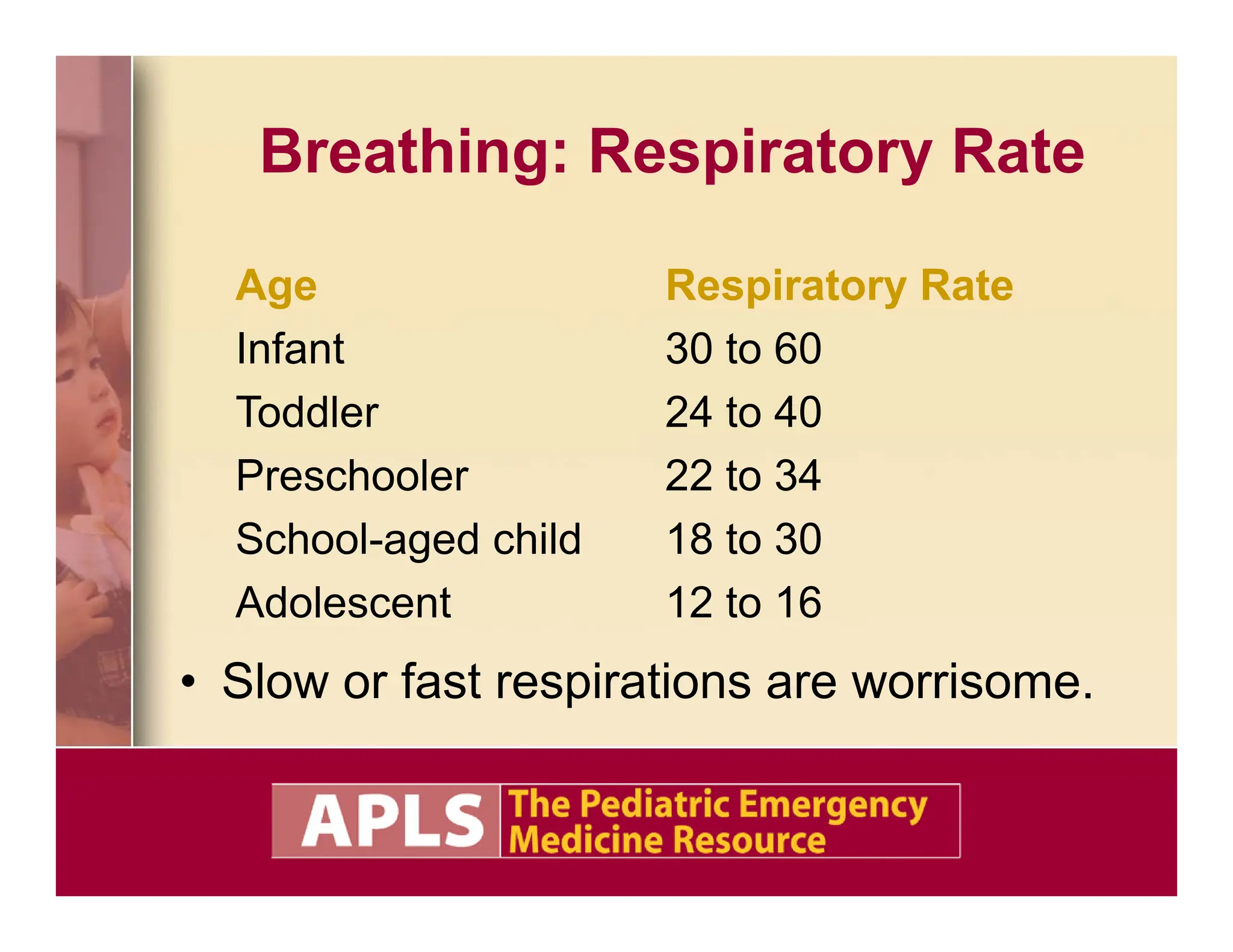
This document outlines pediatric assessment objectives and focuses on the Pediatric Assessment Triangle (PAT) which evaluates appearance, breathing, and circulation to form a general impression of a child's health. It includes multiple case studies illustrating pediatric emergency scenarios and management priorities, emphasizing the importance of ongoing assessment and tailored approaches based on age-specific features. Essential guidelines for evaluating and treating respiratory distress, shock, and other conditions in children are also presented.