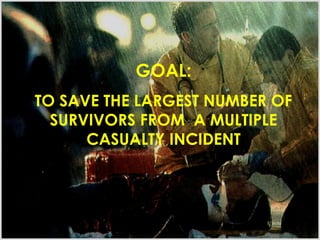
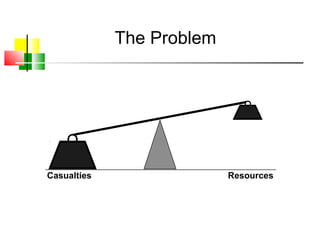
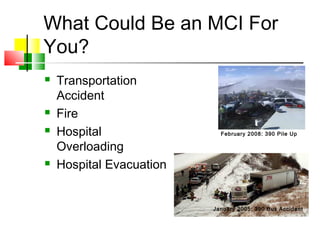
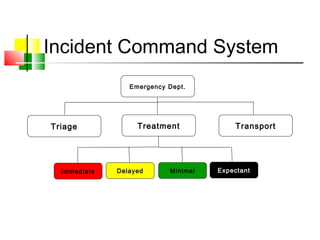
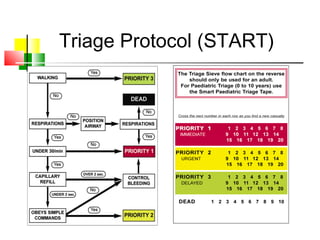
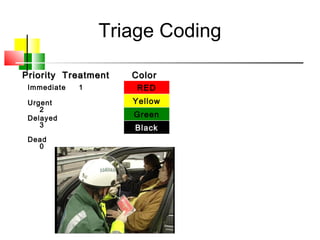
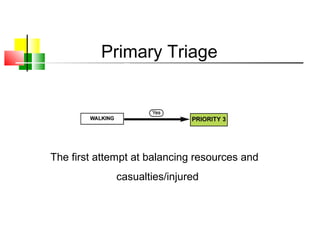
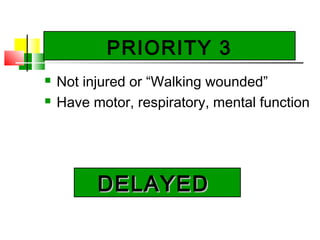
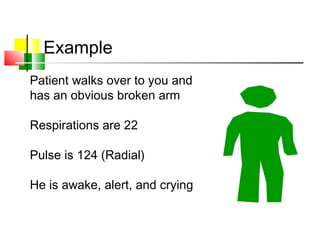
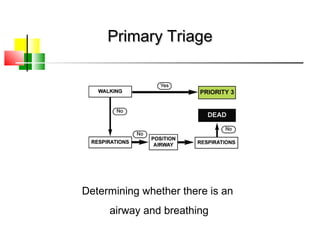
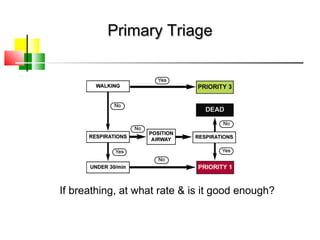
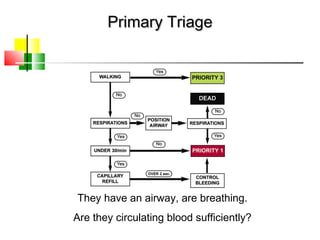
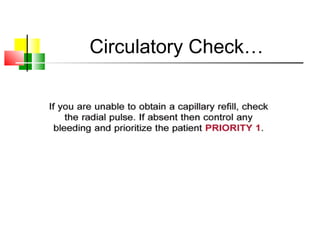
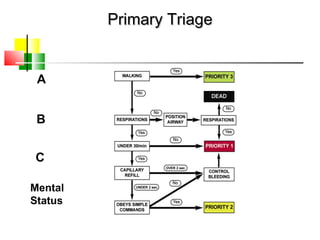
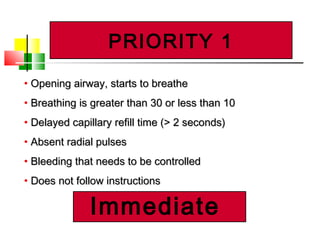
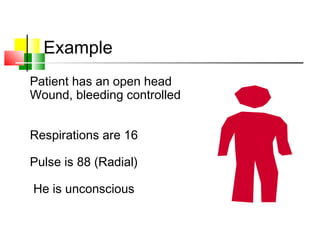
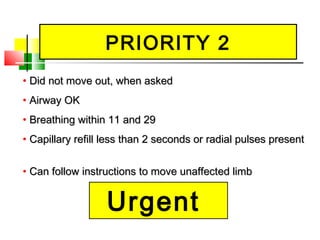
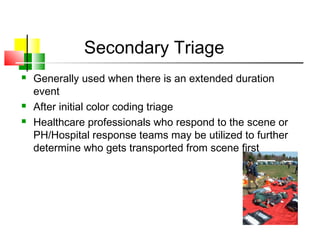
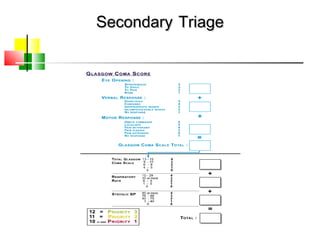
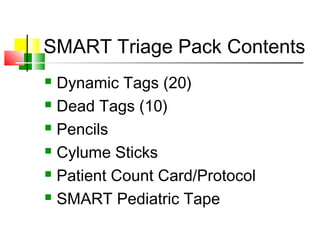
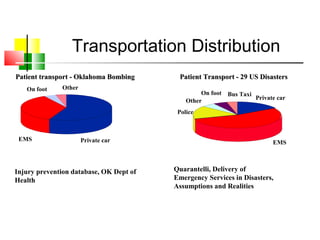
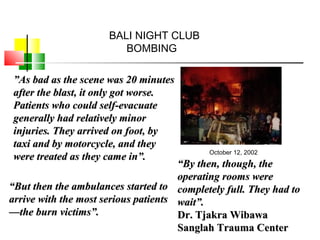
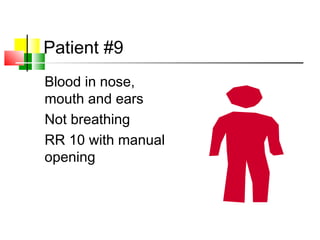
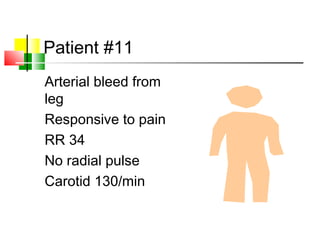
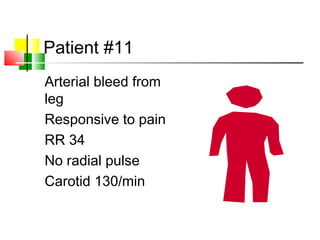
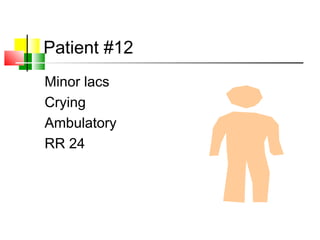
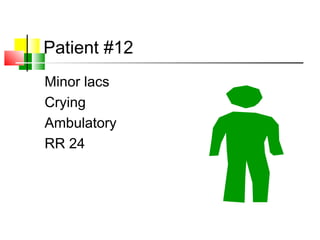
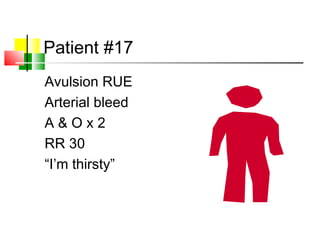
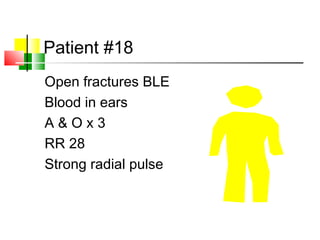
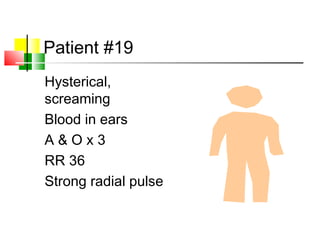
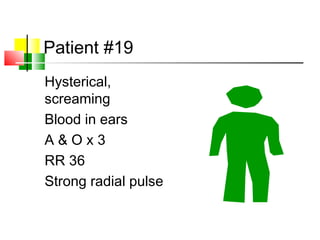
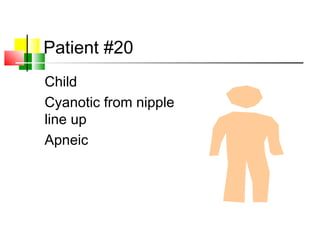
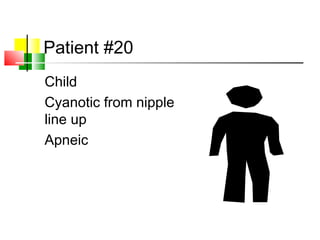
This document discusses disaster triage and managing mass casualty incidents. It defines a mass casualty incident as an event that overwhelms local medical resources. The goal of disaster triage is to save the largest number of survivors. Different types of triage are discussed, including primary triage on scene and secondary triage during transport or at the hospital. The START triage protocol is presented, which codes patients as immediate, delayed, or expectant based on airway, breathing, circulation, and mental status. The document reviews pediatric triage and the SMART tag triage system. Scenarios are provided to practice triaging multiple patients from a simulated mass casualty event. The goal of disaster triage training is to increase