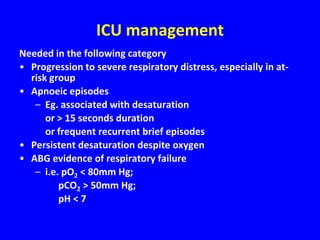
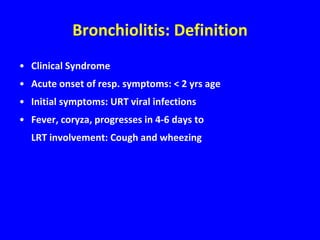
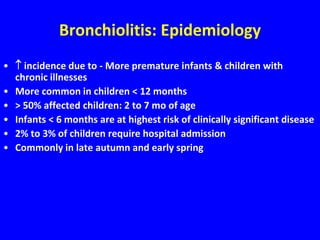
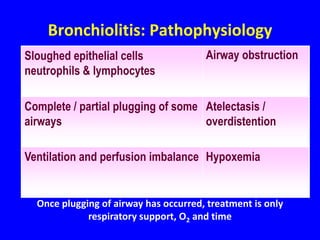
Bronchiolitis is a common respiratory infection in children under 2 years old caused by viruses like respiratory syncytial virus. It presents with symptoms of cough, wheezing, difficulty breathing and feeding. Risk factors include premature birth, exposure to tobacco smoke and attendance at daycare. Diagnosis is clinical and treatment is supportive with oxygen, fluids and respiratory support if severe. Prevention focuses on handwashing and palivizumab prophylaxis in high risk infants to reduce spread of the virus. Prognosis is generally good even in high risk groups though complications can include respiratory failure.



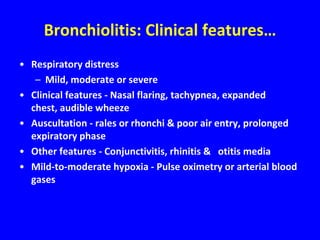
![Bronchiolitis: Clinical features
• Quite variable
• Nasal obstruction with or without rhinorrhea
• Cough - First irritating tight cough
• Poor feeding after the initial onset of symptoms
• Apnea upto 20% in < 12 months with RSV
• Fever - higher than 39oC [adenovirus or influenza]](https://image.slidesharecdn.com/4-bronchiolitis-121027041651-phpapp01/85/4-bronchiolitis-8-320.jpg)