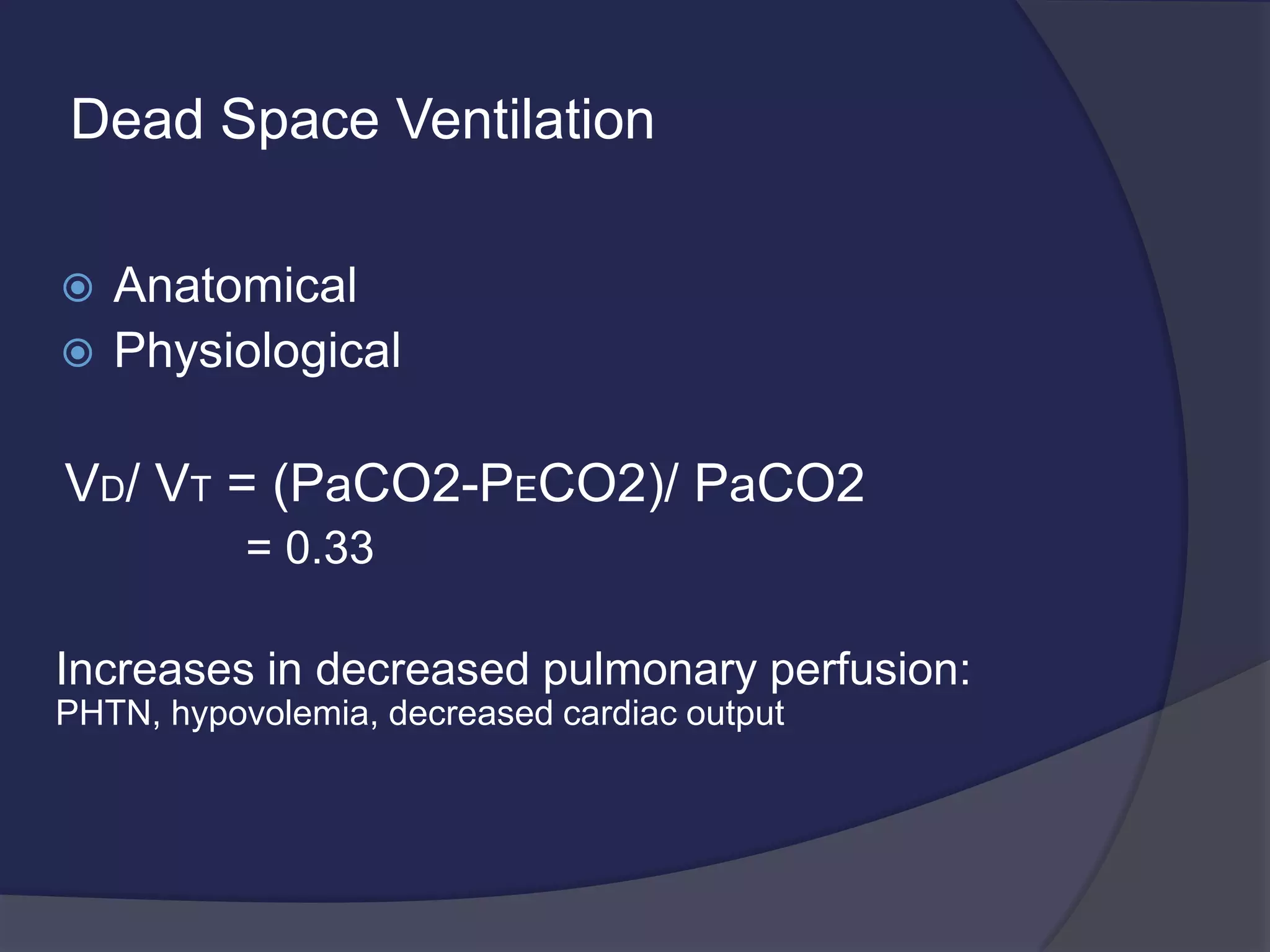
This document discusses respiratory distress and respiratory failure. Respiratory distress refers to increased work of breathing, while respiratory failure is the inability of the lungs to provide oxygen or remove carbon dioxide. Respiratory failure can be acute or chronic. It can occur due to problems with the respiratory pump (central nervous system issues, muscle weakness) or due to airway/lung dysfunction (conditions affecting gas exchange like asthma, pneumonia). Proper monitoring of patients with respiratory distress or failure includes clinical examination, blood gas analysis, and oximetry. Immediate treatment of acute respiratory failure focuses on oxygenation and ventilation. Chronic respiratory failure often has a more insidious onset and requires careful monitoring, especially during sleep or illness.









![Alveolar Gas Composition
PAO2 = PIO2 – (PCO2/R)
PIO2 = (BP – PH2O) . Fio2
PAO2 = [(BP – PH2O) . Fio2] – (PCO2/R)
](https://image.slidesharecdn.com/respiratoryfailure-131030100719-phpapp01/75/Respiratory-failure-in-children-12-2048.jpg)