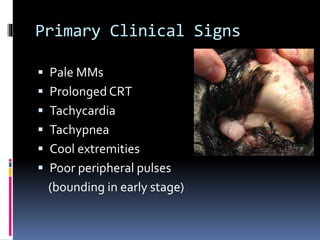
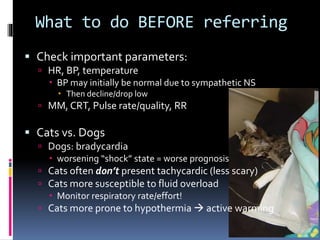
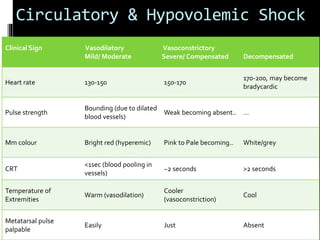
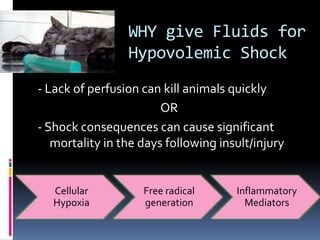
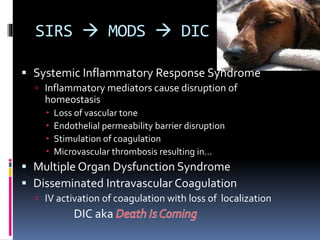
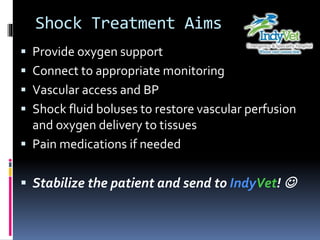
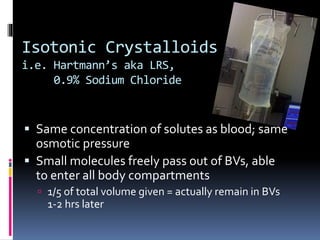
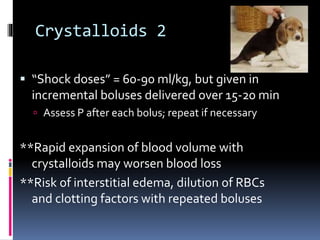
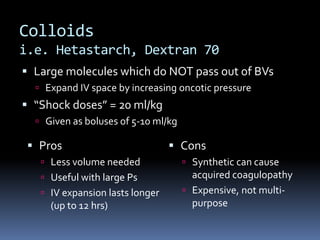
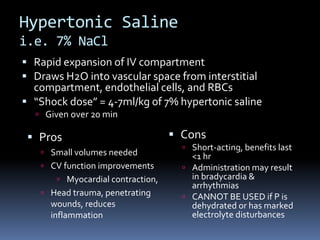
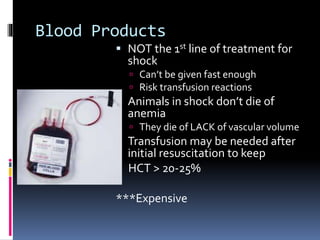
Hypovolemic shock is a condition characterized by inadequate blood volume to deliver oxygen to tissues, often resulting from dehydration or blood loss. Key clinical signs include tachycardia, pale mucous membranes, and hypotension, necessitating prompt assessment and fluid therapy to restore vascular perfusion. Treatment options include isotonic crystalloids, colloids, and hypertonic saline, with a focus on patient stabilization and careful monitoring.