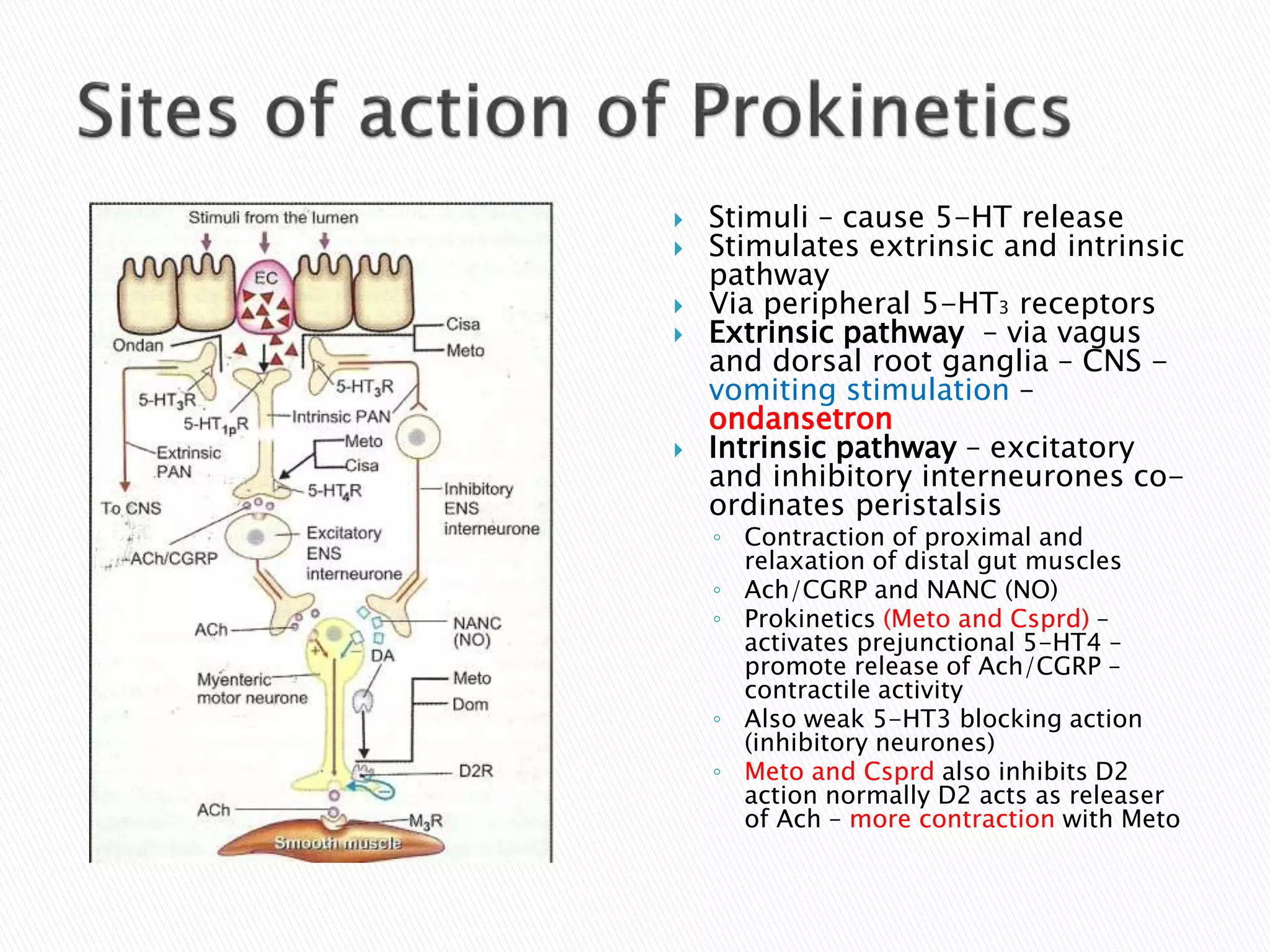
The document discusses the mechanisms and pharmacology of vomiting and its treatment, highlighting the emetic response and the role of various neurotransmitters and receptors involved in this process. It outlines different emetic agents and medications that can induce or prevent vomiting, including their mechanisms of action, indications, dosing, and adverse effects. Additionally, it categorizes drugs based on their use in conditions like motion sickness, chemotherapy-induced nausea, and other vomiting disorders.