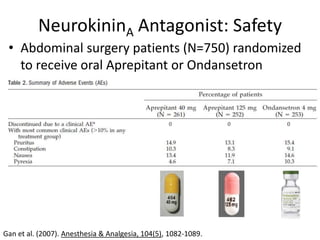
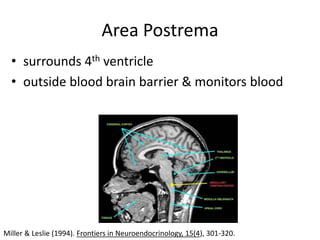
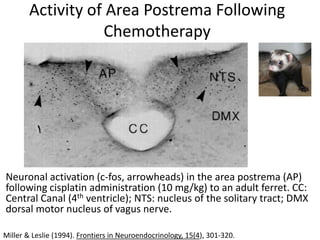
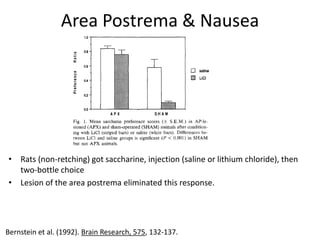
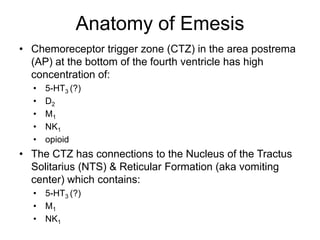
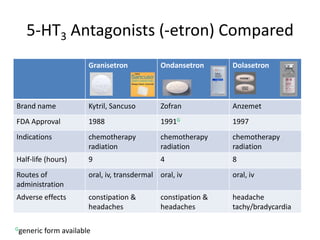
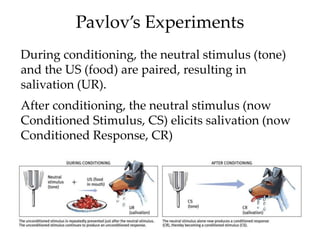
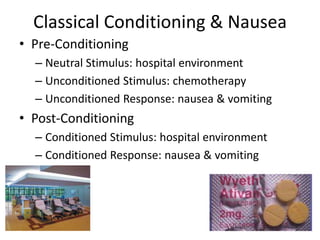
The document outlines the mechanisms and classifications of antiemetic agents and their role in managing nausea and vomiting, particularly in the context of chemotherapy and other medical treatments. It details specific drug targets, mechanisms of action, and adverse effects of various antiemetics, such as 5-HT3 antagonists and neurokinin-1 antagonists. Additionally, it highlights the importance of the chemoreceptor trigger zone in the emesis pathway and the interplay between conditioning and nausea responses.













![Density of Cannabinoid Receptor 1 (Increased
Darkness = more receptors labeled with [3H]CP-55,940)
Hekenham et al. (1991) J Neurosci, 11, 563-583.](https://image.slidesharecdn.com/antiemetics-121002074836-phpapp02/85/Antiemetics-24-320.jpg)