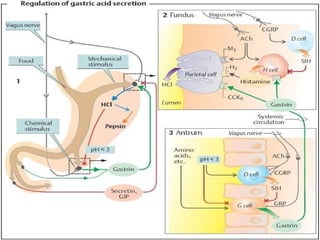
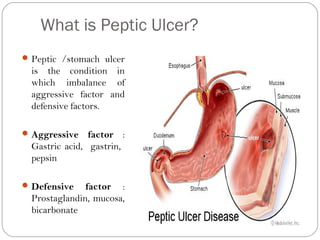
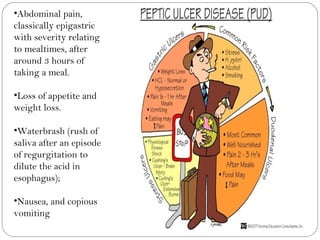
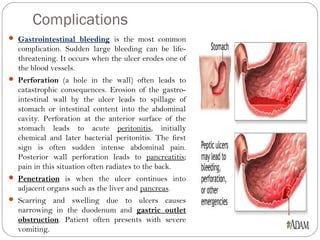
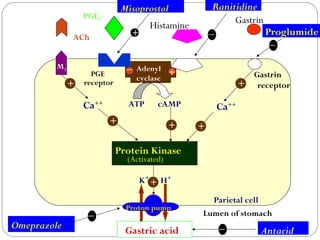
1) Peptic ulcers are caused by an imbalance between aggressive factors like gastric acid and protective factors in the stomach and duodenum.
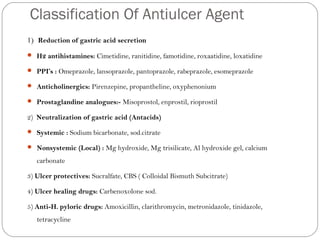
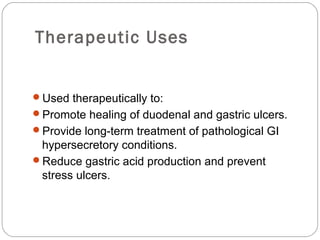
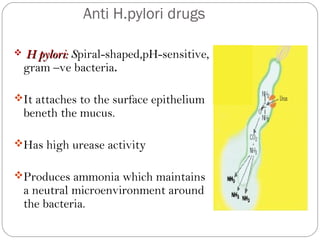
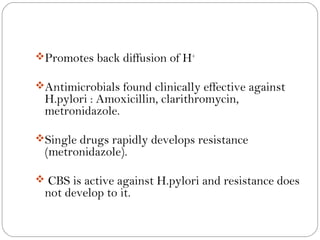
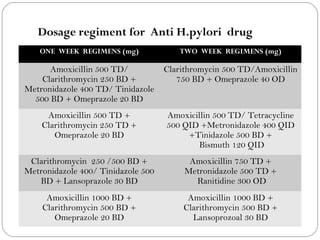
2) Anti-ulcer drugs work by decreasing gastric acid secretion, enhancing mucosal protection, or eradicating the H. pylori bacteria responsible for many ulcers.
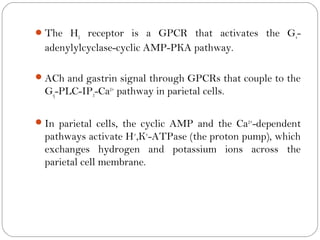
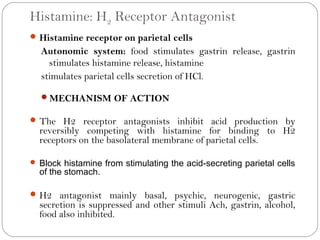
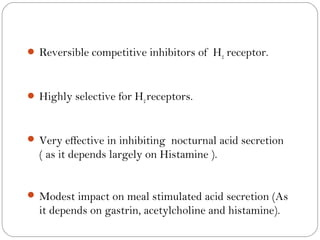
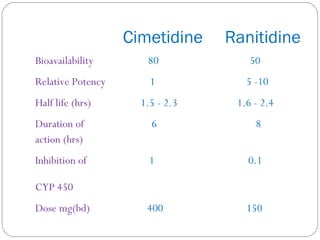
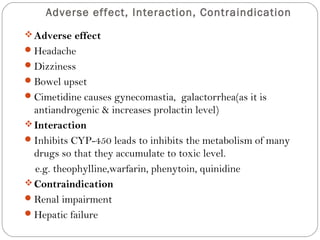
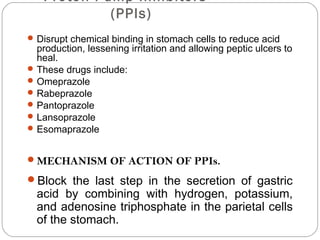
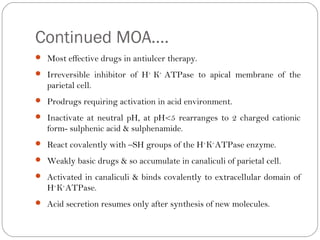
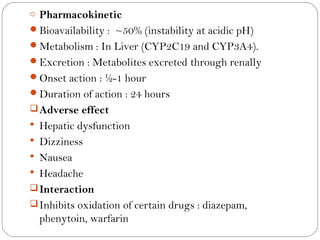
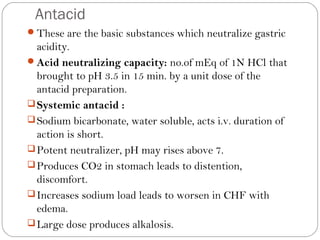
3) Common classes of anti-ulcer medications include H2 receptor antagonists, proton pump inhibitors, antacids, and anti-H. pylori drugs. H2 receptor antagonists and proton pump inhibitors reduce acid by blocking histamine and the proton pump, while antacids neutralize existing acid.