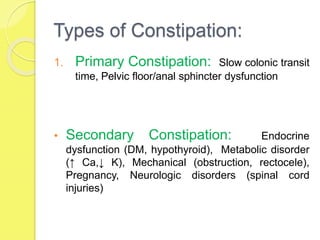
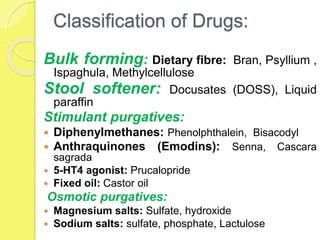
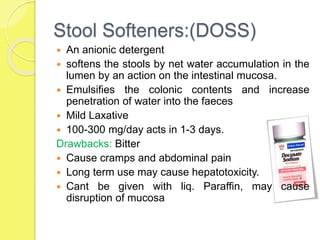
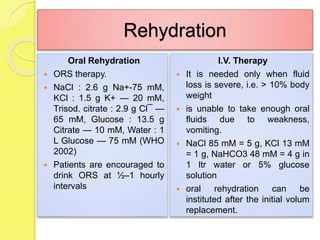
The document discusses the conditions of constipation and diarrhea, detailing their definitions, causes, risk factors, and treatment options. It categorizes drugs used for treating these conditions, including laxatives, purgatives, and rehydration therapies. Additionally, it emphasizes the importance of dietary fiber, hydration, and various pharmacological interventions for relief and management.