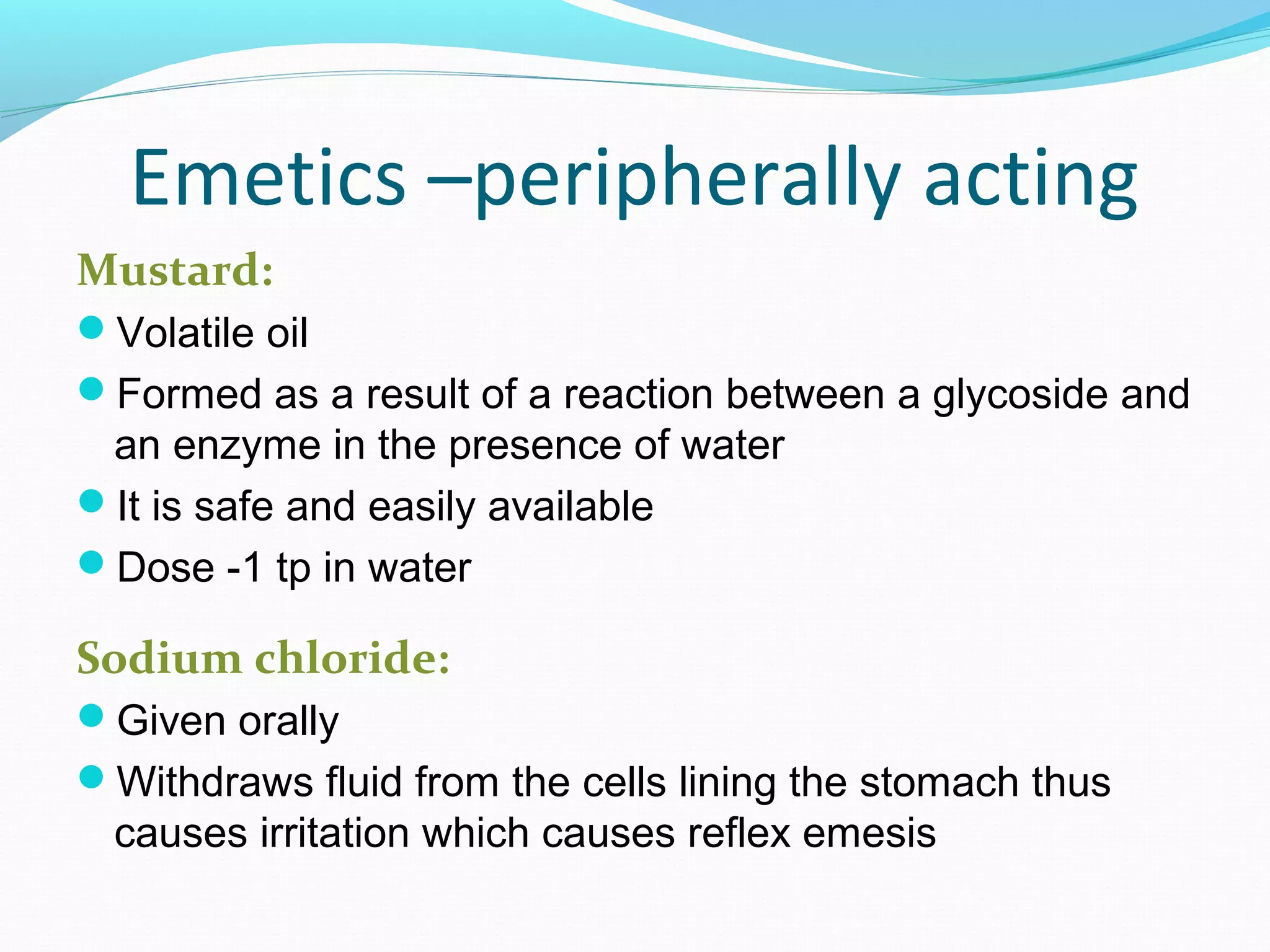
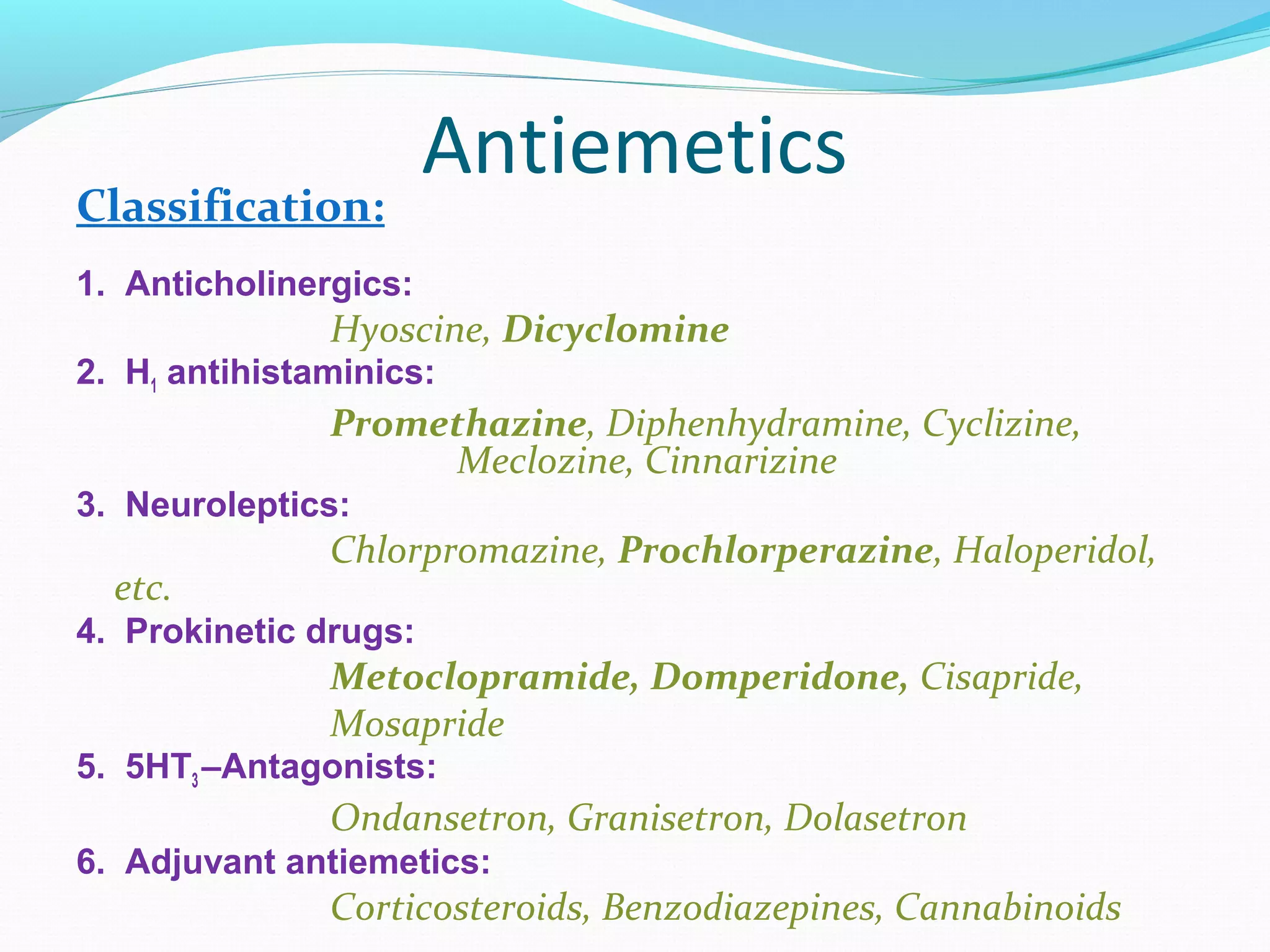
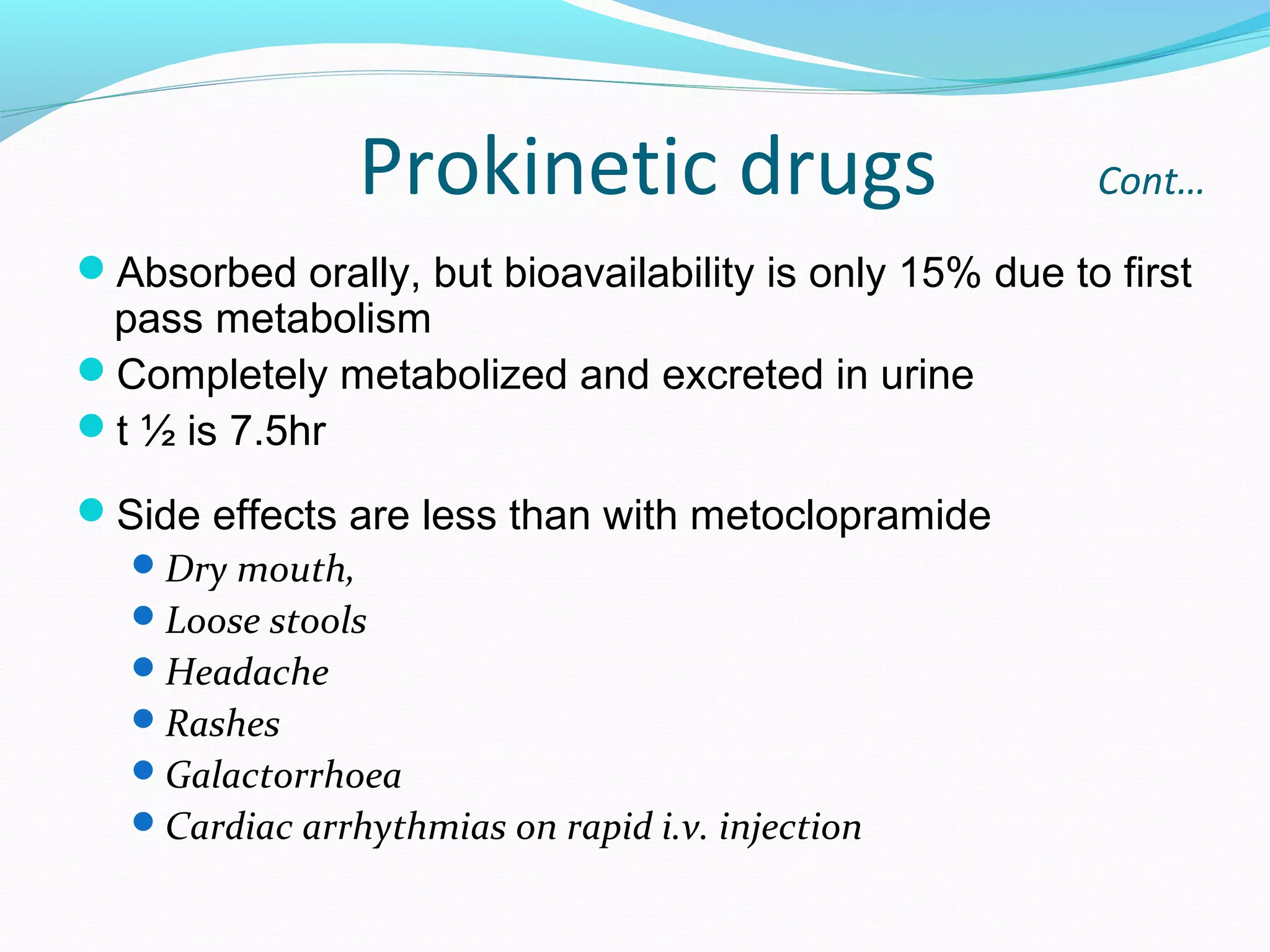
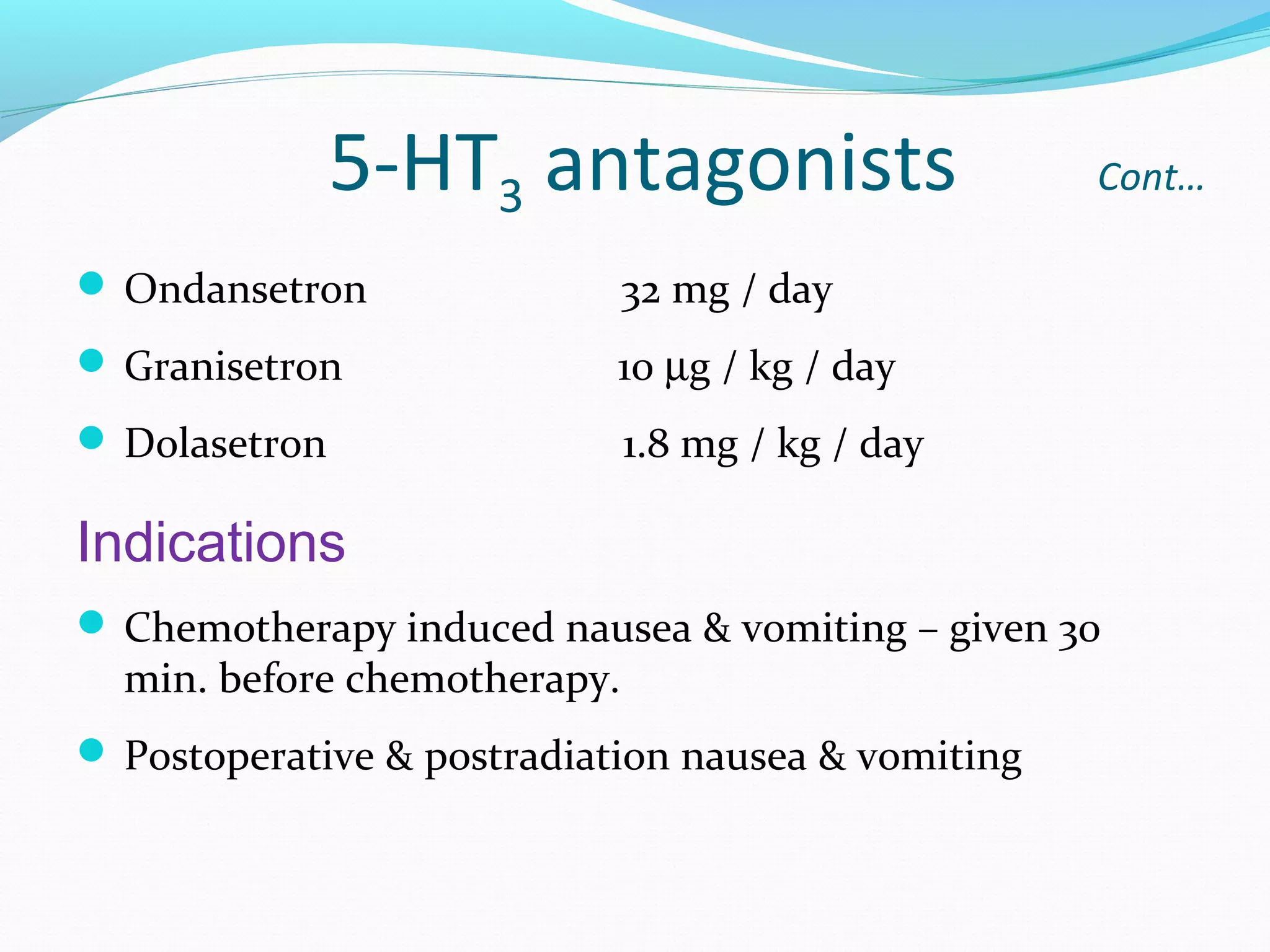
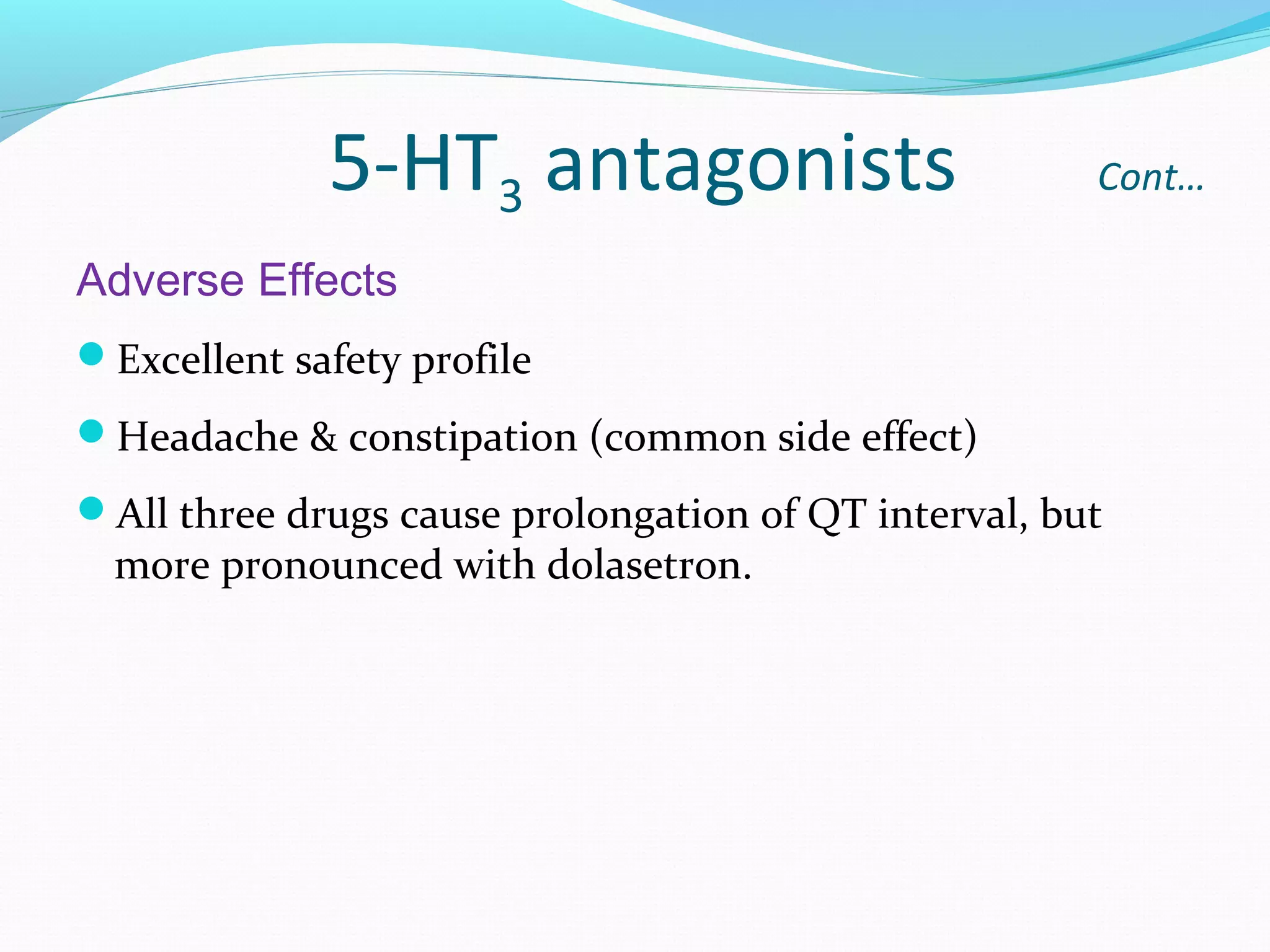
This document discusses emesis (vomiting) including its pathophysiology and treatment. It notes that emesis is a protective mechanism that eliminates harmful substances via stimulation of the emetic center in the medulla oblongata. Multiple pathways can trigger vomiting including the chemoreceptor trigger zone and nucleus tractus solitarius, which are important relay areas. Emetics and antiemetics are then described. Emetics include apomorphine, mustard, and ipecacuanha, while antiemetics include anticholinergics, H1 antihistamines, neuroleptics, prokinetic drugs, 5-HT3 antagonists, and adjuvant medications. Various drugs that